JACC:OCT vs. 血管造影指导的PCI
2018-08-02 国际循环编辑部 国际循环
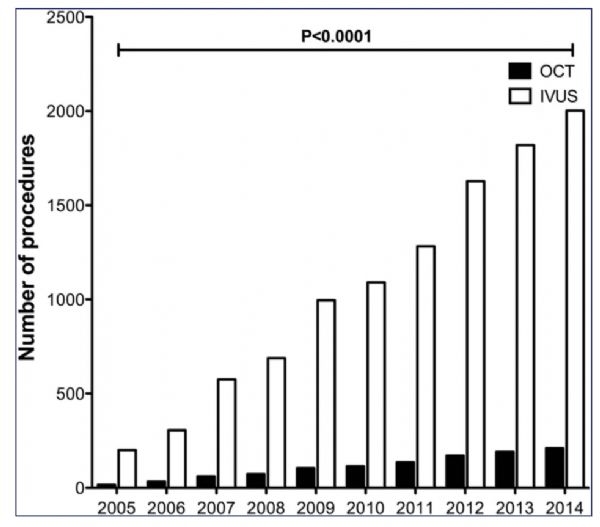
血管造影指导的经皮冠状动脉介入治疗(PCI)具有一定局限性,迄今为止有关其对临床终点影响的数据有限,但光学相干断层扫描(OCT)的空间分辨率优势可转化为有意义的临床获益。JACC发表的一项最新研究探讨了在PCI时使用OCT对患者长期生存的影响。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
51
血管造影指导的PCⅠ。
118
不错耶,学习了
122
血管造影指导的pci
104
#OCT#
53
#ACC#
52
#造影#
75
学习了受益匪浅
119
学习了,学习了
100
学习学习再学习
47