掌中“包”别大意!腱鞘巨细胞瘤迎来最佳治疗药物Turalio
2019-08-08 佚名 汉鼎好医友
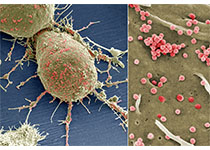
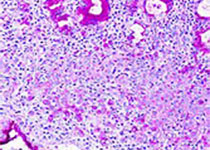
手上长肿物,最常见的是腱鞘囊肿,早期通过按压即可消除。但掌中“包”也可能是一种罕见肿瘤--腱鞘巨细胞瘤,切莫大意,按压不仅无济于事,反而可能激惹包块,加重病变。近日,美国FDA批准Turalio(Pexidartinib)胶囊用于治疗成人手术后无改善的症状性腱鞘巨细胞瘤(TGCT)。这是FDA批准的第一个治疗这种罕见疾病的疗法。FDA肿瘤卓越中心主任、药物评估和研究中心血液和肿瘤产品办公室代理主任

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Turalio#
71
#腱鞘巨细胞瘤#
53
#治疗药物#
70
#细胞瘤#
86
#巨细胞#
64