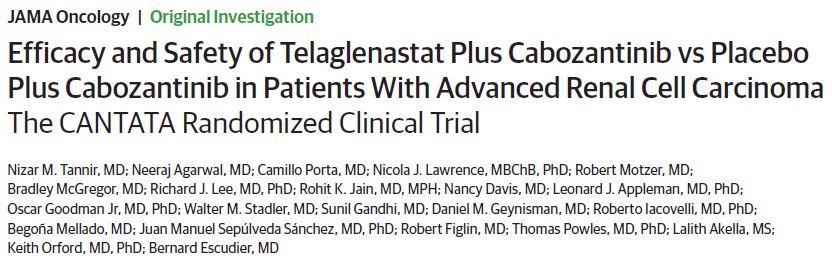
JAMA Oncol:Telaglenstat联合卡博替尼治疗转移性晚期肾细胞癌
2022-09-09 MedSci原创 MedSci原创
Telaglenstat未能改善卡博替尼对转移性晚期肾细胞癌患者的疗效
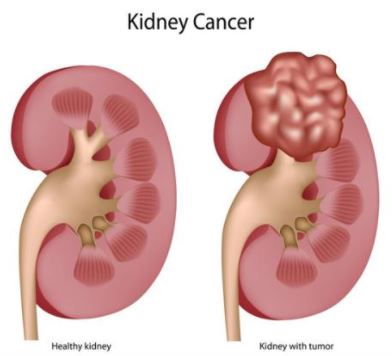
代谢失调是肾细胞癌 (RCC) 的标志。谷氨酰胺酶是一种关键酶,通过将谷氨酰胺转化为谷氨酸来促进肿瘤生长。Telaglenstat 是一种研究性、一线、选择性、口服谷氨酰胺酶抑制剂,可阻断谷氨酰胺利用和下游途径。在临床前试验中,Telaglenstat与卡博替尼在RCC模型中表现出了协同作用。
CANTATA研究旨在比较Telaglenstat联合卡博替尼(Tela+Cabo)和安慰剂联合卡博替尼(Pbo+Cabo)在晚期RCC患者中的疗效和安全性。
这是一项随机、安慰剂为对照、双盲的飞行试验,招募了晚期肾透明细胞癌患者,随机(1:1)分成两组,接受口服卡博替尼(60 mg/天)+Telaglenstat(800 mg*2次/天)或安慰剂治疗直到病情进展或出现不可耐受的毒性。主要终点是无进展生存期。
共招募了444位患者:Tela+Cabo组 221位(中位年龄 61岁,21%的女性),Pbo+Cabo组 223位(中位年龄 62岁,30%的女性)。共276位(62%)患者既往接受过免疫检查点抑制剂治疗,包括128位接受过纳武单抗+伊匹单抗治疗的患者,其中93位未接受过抗血管生成治疗。
两组的PFS和OS
Tela+Cabo组和Pbo+Cabo组的中位无进展生存期分别是9.2个月和9.3个月(HR 0.94, P=0.65)。Tela+Cabo组和Pbo+Cabo组的总缓解率分别是31%和28%。
两组的不良事件发生情况
两组的治疗相关不良反应事件发生率相近。Tela+Cabo组和Pbo+Cabo组3-4级治疗相关不良事件的发生率分别是71%和79%,包括高血压(17% vs 18%)和腹泻(15% vs 13%)。Tela+Cabo组和Pbo+Cabo组分别有23位(10%)和33位(15%)患者因不良反应停用卡博替尼。
总之,该研究结果显示,Telaglenstat未能改善卡博替尼对转移性晚期肾细胞癌患者的疗效。
原始出处:
Tannir NM, Agarwal N, Porta C, et al. Efficacy and Safety of Telaglenastat Plus Cabozantinib vs Placebo Plus Cabozantinib in Patients With Advanced Renal Cell Carcinoma: The CANTATA Randomized Clinical Trial. JAMA Oncol. Published online September 01, 2022. doi:10.1001/jamaoncol.2022.3511
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
97
#转移性晚期#
75
#NST#
102
#细胞癌#
69
#转移性#
83
#晚期肾细胞癌#
136