Neurology:血管周围空间可有效反映帕金森的运动障碍
2021-03-22 Freeman MedSci原创
血管周围空间可有效反映帕金森的运动障碍
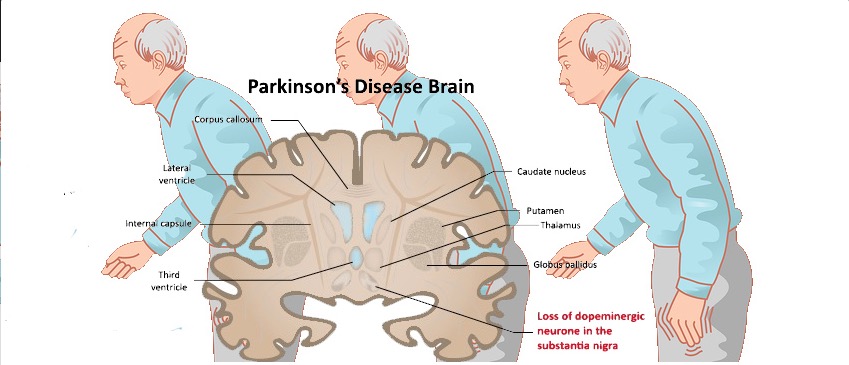
血管周围空间(PVSs)是围绕着大脑小穿孔血管的间质性液体填充腔,在传统的脑磁共振成像(MRI)中,年轻的大脑通常看不到PVSs;然而,随着年龄的增长,扩大的PVSs会在特定的大脑区域(如基底神经节、半卵圆形中心和海马)变得更多,这些PVSs呈线性或卵圆形结构,信号强度与脑脊液相似。扩大的PVSs的临床意义仍有争议:一些研究表明,扩大的PVSs是老年人的正常现象,而另一些研究则指出,MRI可见的PVS,尤其是基底节(BG)的PVSs,与脑小血管疾病、炎症和认知障碍密切相关。
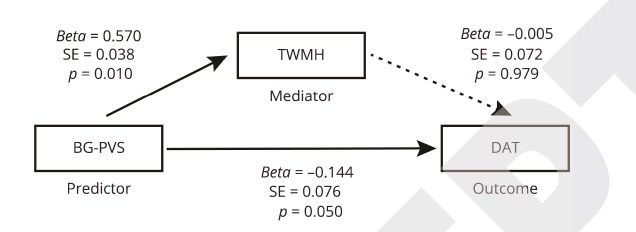
此外,最近的证据表明,PVSs是淋巴系统的一部分,通过该系统清除大脑中的有害代谢物,因此,淋巴途径的功能障碍可能会导致PVSs的扩大以及蛋白质聚集在大脑中的积累,这表明扩大的PVSs与蛋白质错误折叠疾病(如阿尔茨海默病和帕金森病)之间可能存在联系。
到目前为止,扩大的PVSs在PD中的临床相关性很少被报道。考虑到黑质变性是PD的核心病理特征,基底节的PVS(BG-PVS)扩大可能比其他部位的PVS更具有临床相关性,一些病例报告提出,扩大的BGPVS可能转化为PD患者的帕金森病和非典型临床特征。最近的研究表明,可见BG-PVS与PD的认知功能下降有关,然而,扩大的BG-PVS对PD的长期运动结果的影响尚未得到评估。
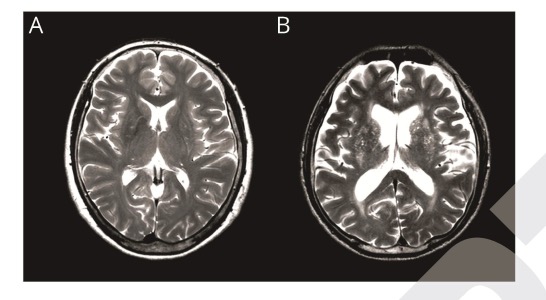
PVS 示意图
藉此,韩国高丽大学的Seok Jong Chung等人,探究了基线时基底节PVS(BG-PVS)是否与以下指标的关系:左旋多巴诱导的运动障碍(LID)步态冻结(FOG)和多巴胺能药物剂量的增加。
他们分析创尔248名接受脑MRI和多巴胺转运体(DAT)扫描的药物无反应早期PD患者(随访>3年,平均年龄67.44±8.46岁,130名女性)。在轴向T2加权图像上统计基线扩大的BG-PVSs数量。然后,患者被分为两组:PD组具有低数量(0-10)的扩大PVSs(PD-EPVS-; n = 156)和具有高数量(>10)的扩大PVSs(PD-EPVS+; n = 92)。
并使用Cox回归模型比较了组间左旋多巴诱导的运动障碍(LID)、无步态冻结(FOG)的时间。最后使用线性混合模型比较了组间单位体重左旋多巴等效剂量的纵向增加。
他们发现,PD-EP中的患者 PD-EPVS+组的患者年龄较大(72.28±6.07岁),小血管疾病负担比PD-EPVS-组的患者(64.58±8.38岁)更大。
PD-EPVS+组在除腹侧纹状体外的所有纹状体亚区表现出更严重的DAT可用性下降。PD-EPVS+组发生FOG的风险较高,但组间LID的风险相当。
与PD-EPVS-组相比,PD-EPVS+组需要更高剂量的多巴胺能药物才能有效控制症状。
这个研究的重要意义在于,发现了基线扩大的BG-PVSs可以作为PD运动障碍进展的指标。
原文出处:
Perivascular Spaces in the Basal Ganglia and Long-term Motor Prognosis in Newly Diagnosed Parkinson Disease
Seok Jong Chung, Han Soo Yoo, Na-Young Shin, Yae Won Park, Hye Sun Lee, Ji-Man Hong, Yun Joong Kim, Seung-Koo Lee, Phil Hyu Lee, Young H. Sohn
Neurology Mar 2021, 10.1212/WNL.0000000000011797; DOI: 10.1212/WNL.0000000000011797
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Neurol#
88
感谢分享!
104
感谢好文!
101
#运动障碍#
0
学习
223
为啥还不结束
114