Cancer Med:国内多中心随机双盲II期研究表明安罗替尼(Anlotinib)后线治疗较安慰剂改善晚期或转移性食管鳞癌患者的预后
2021-12-29 yd2015 MedSci原创
研究表明,与安慰剂相比,在既往治疗过的复发或转移性ESCC患者中使用安罗替尼(Anlotinib)显著改善无进展生存期(PFS)。
安罗替尼(Anlotinib)是一种口服小分子酪氨酸激酶抑制剂(TKI),靶向血管内皮生长因子(VEGF)受体1、2和3,成纤维细胞生长因子(FGF)受体1-4、血小板衍生生长因子(PDGF)受体ɑ和β、Ret和c- Kit。因此,来自北京协和医院的团队联合国内多家医院开展了相关研究,评估安罗替尼二线或后线治疗晚期或转移性食管鳞癌(ESCC)患者的疗效和安全性。相关结果发表在Cancer Medicine杂志上。
这项随机、双盲、安慰剂对照的II期临床试验在中国13家医院进行(ALTER1102 ,NCT02649361)。符合条件的患者为经组织学证实的复发或转移性食管鳞癌患者,至少有一个可测量病灶,ECOG 0-2分,既往曾接受化疗,随机分配(2:1)在第1 - 14天接受口服anlotinib 12mg或安慰剂(每21天重复一次)。主要终点为无进展生存期(PFS);次要研究终点是OS,客观缓解率(ORR),疾病控制率(DCR)和安全性。
在2016年1月6日-2018年5月22日期间,共对196名患者进行了资格筛选。共有165名患者被随机(2:1)分配到anlotinib组(n = 110)或安慰剂组(n = 55)。164例患者开始接受治疗,其中109例接受anlotinib治疗,55例接受安慰剂治疗。anlotinib组患者的中位年龄为62岁,安慰剂组患者的中位年龄为61岁。大多数患者为男性以及ECOG评分为1分。在两组患者中,64%的患者以前接受过两种或两种以上的化疗。患者既往接受过肿瘤手术的比例,anlotinib组为79%,安慰剂组为60%。
研究者评估的中位无进展生存期(PFS):anlotinib组为3.02个月(95% CI 2.63-3.65),安慰剂组为1.41个月(95% CI 1.38-1.41)。 Anlotinib组较安慰剂组明显延长患者的PFS (HR 0.46 [95% CI 0.32– 0.66]; p < 0.001)。与研究者评估结果一致,通过盲法中心回顾评估,anlotinib组的中位PFS为2.83个月(95% CI 2.30-3.61),而安慰剂组的中位PFS为1.41个月(95% CI 1.38-1.41) (HR 0.43 [95% CI 0.30 0.62];p<0.001)。亚组分析也观察到anlotinib治疗较安慰剂组获益。
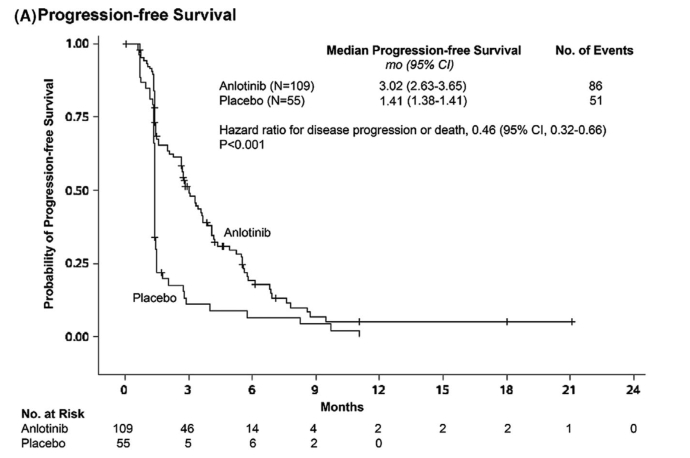
两组的PFS差异以及亚组分析
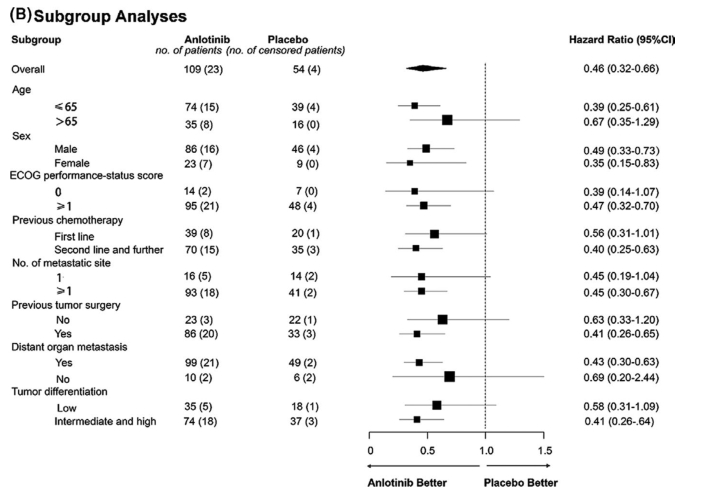
两组间OS无统计学差异(HR 1.18 [95% CI 0.79 1.75];p = 0.426)。Anlotinib组的中位OS为6.11个月(95% CI 4.40-7.79),安慰剂组为7.20个月(95% CI 4.83-8.38)。校正不平衡的手术史后,HR和log- rank p值分别为1.24 (95% CI 0.82 1.88)和0.2989。
两组的OS差异
两组的ORR无显著差异(8/109(7.3%) vs 2/55(3.6%);p = 0.498)。Anlotinib组的DCR显著高于安慰剂组(64% vs. 18%,p<0.001); Anlotinib组患者病情稳定的比例更高(57% vs 15%)。
两组任何级别治疗相关AEs发生率分别为94%和82%。最常见的是疲劳 (57% vs. 35%), 高血压(54% vs. 16%), 纳差(43% vs. 25%),和甲减(36% vs. 5%)。3-4级AEs分别为37%和11%。两组治疗相关严重AEs发生率分别为19%和2%。

AEs
综上,研究表明,与安慰剂相比,在既往治疗过的复发或转移性ESCC患者中使用安罗替尼(Anlotinib)显著改善无进展生存期(PFS)。
原始出处:
Huang J, Xiao J, Fang W, Lu P, Fan Q, Shu Y, Feng J, Zhang S, Ba Y, Zhao Y, Liu Y, Bai C, Bai Y, Tang Y, Song Y, He J. Anlotinib for previously treated advanced or metastatic esophageal squamous cell carcinoma: A double-blind randomized phase 2 trial. Cancer Med. 2021 Mar;10(5):1681-1689. doi: 10.1002/cam4.3771. Epub 2021 Feb 14. PMID: 33586360; PMCID: PMC7940231.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#多中心#
108
#鳞癌患者#
74
#安慰剂#
100
#转移性#
84
#食管#
70
#鳞癌#
76
#双盲#
90
#Med#
58
学习。
82