Radiology:前交叉韧带损伤后,膝关节有何结构性改变?
2021-07-23 shaosai MedSci原创
前交叉韧带(ACL)撕裂与膝关节骨关节炎(OA)进展的风险增加相关。ACL重建术通常是为了提高膝关节的稳定性,并降低半月板或软骨的损伤以及膝关节OA发生的风险。
前交叉韧带(ACL)撕裂与膝关节骨关节炎(OA)进展的风险增加相关。ACL重建术通常是为了提高膝关节的稳定性,并降低半月板或软骨的损伤以及膝关节OA发生的风险。但是,在ACL损伤后约10–20年,无论采用何种治疗方法,仍约有10%–90%的患者会发生膝关节OA。ACL损伤后OA发生风险增加的驱动机制尚不确定,但人们普遍认为多种因素均会影响发生创伤后OA的可能性。这些因素包括损伤的严重程度、涉及的关节组织、损伤时的年龄以及损伤发生的时间等。
炎症、半月板病变、半月板切除术,外伤性软骨损伤的存在以及有或没有关节表面破坏的骨髓病变(BML)均可以进一步引起多组织的改变。X线及CT检查一只在出现明显的骨适应性改变后才能显示出骨关节炎关节的晚期变化。然而多项研究表明,MRI可用于评估ACL损伤后关节结构的早期改变,但目前尚无关于比较不同治疗方法长期数据的相关报道及研究。
近日,发表在Radiology杂志的一项研究在ACL损伤后的5年内,通过使用MRI对包括软骨、BML、骨赘和炎性标志物等结构性关节损伤进行了评估,并比较了此类组织损伤的发生频率与非手术及手术治疗的关系,为临床阐明ACL损伤后组织结构的发展机制一公里参考依据,为进一步的早期诊断及治疗提供了技术支持。
本项研究为前瞻性试验(ISRCTN 84752559)的二次分析。共评估了119名急性ACL损伤患者。研究对象于2002年至2006年入组,2008年开始2年随访,2011年开始5年随访。在基线、2年和5年时进行了随访1.5 T MRI检查。根据一个有效的评分工具对MRI扫描进行读取。使用Kruskal-Wallis测试评估三组之间结构损伤的频率是否不同。
对119名参与者(平均年龄26岁±5 [标准差])中的91名男性进行了评估。在2年和5年的随访中,分别有13%和13%的膝关节表现出内侧胫股关节的软骨损伤,11%和17%的膝关节表现出外侧胫骨关节的软骨损伤,有4%和8%的膝关节出现了髌骨关节的软骨损伤。内侧胫骨关节的骨赘发育占23%和29%,外侧胫骨关节的骨赘发育占36%和43%,髌骨关节占35%和37%。在2年或5年时,两组之间软骨损伤发生或恶化的、骨髓损伤和骨赘方面均没有显著差异。仅康复组在2年(P = .02)和5年(P = .008)随访时表现出少量的霍法氏滑膜炎。
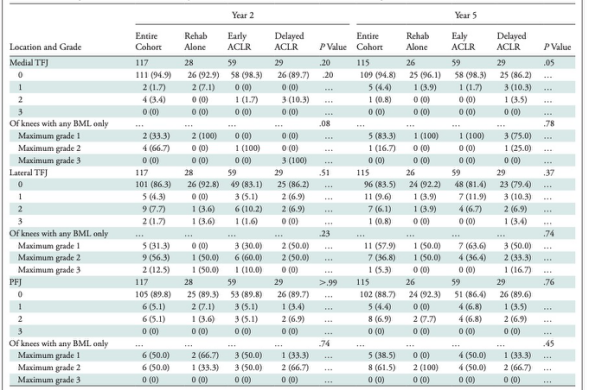
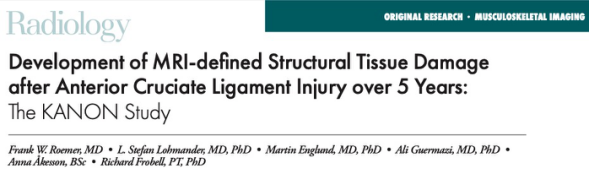
表1 软骨损伤的发生和进展。

表2 骨赘的发生和进展。
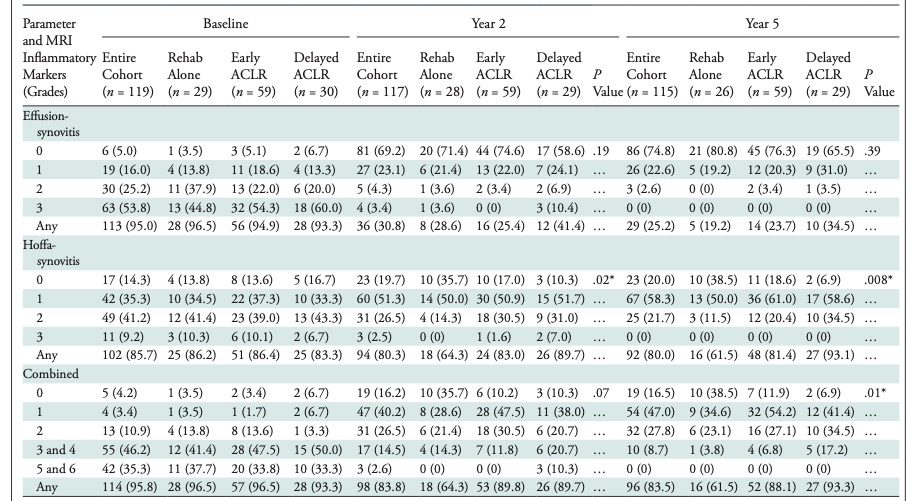
表3 MRI炎症标记物。
本研究发现,软骨损伤最常发生在外侧胫股关节,是最常受严重急性创伤性结构损伤影响的位置。退行性骨髓病变(BMLs)的发展在损伤2年及5年时十分罕见,而且在外侧胫股关节的发生率明显高于其它位置。骨赘的形成在所有位置中均十分常见,并且这些骨赘的体积大多很小。本研究同时发现,无论采取何种治疗措施,大多数的膝关节结构变化都出现在创伤后的头2年。在急性前交叉韧带(ACL)损伤后第2年和5年,软骨损伤、BMLs和骨赘发生率方面在治疗组之间没有显著差异。
原文出处:
Frank W Roemer,L Stefan Lohmander,Martin Englund,et al.Development of MRI-defined Structural Tissue Damage after Anterior Cruciate Ligament Injury over 5 Years: The KANON Study.DOI:10.1148/radiol.2021202954
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#结构性#
81
#损伤#
83
#前交叉韧带#
85
#韧带#
75
好文章,谢谢分享。
90