JACC:肝移植后心脏移植可减轻致敏患者的心脏移植排斥反应!
2021-03-17 Nebula MedSci原创
原位心脏移植仍是晚期心衰的治疗金标准,但显著的同种异体致敏限制了需心脏移植患者获得器官的机会,导致等待时间更长和等待死亡率高。而且,目前的脱敏策略在使移植成功方面的作用有限。
原位心脏移植仍是晚期心衰的治疗金标准,但显著的同种异体致敏限制了需心脏移植患者获得器官的机会,导致等待时间更长和等待死亡率高。而且,目前的脱敏策略在使移植成功方面的作用有限。
本文旨在报道使用一种新的肝后心脏移植(HALT)方案进行心肝联合移植的累积经验。
纳入需要在单一机构进行心脏和肝脏联合移植的高度致敏患者,量身制定肝移植后心脏移植方案。患者被列为双器官患者,由于同种抗体水平高,排斥风险增加或等待时间明显延长。
移植后供者特异性抗体(DSA)
共7例(43±7岁,86%女性)高致敏患者(中位数计算群体反应性抗体=77%)接受了HALT治疗。所有患者均有显著的、不可接受的供者特异性抗体(DSA)(平均荧光抗体>4000)。术前前瞻性流式细胞仪T细胞交叉配型全部为阳性,B细胞交叉配型有5例阳性。
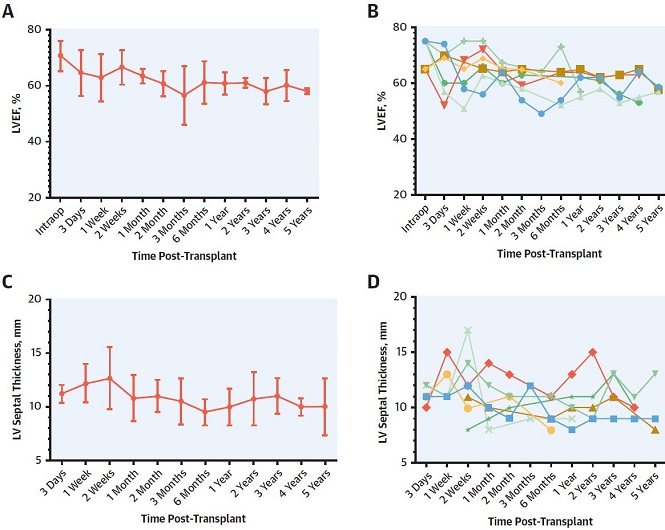
移植后的LVEF和LV间隔厚度
HALT后,回顾性交叉配型(B细胞和T细胞)全部转为阴性。DSA明显降低;在最后一次随访中,所有预先形成或新形成的DSA水平均显著降至2000以下。
中位随访时间为48个月(四分位数范围:25~68个月),无患者发生1R级以上的排斥反应。有1例死于转移性癌症,无明显移植器官功能障碍。
总之,肝后心脏移植方案可通过消除DSA从而使移植获得成功,并能有效地预防心肝联合移植的高度致敏患者的不良免疫学结局。
原始出处:
Daly Richard C,Rosenbaum Andrew N,Dearani Joseph A et al. Heart-After-Liver Transplantation Attenuates Rejection of Cardiac Allografts in Sensitized Patients.J Am Coll Cardiol, 2021, 77: 1331-1340.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
79
#排斥#
70
#ACC#
86
#排斥反应#
76
#心脏移植#
146