如何正确使用感染性指标“CRP、PCT、SAA”
2018-06-05 苏显都 儋州市人民医院 检验医学
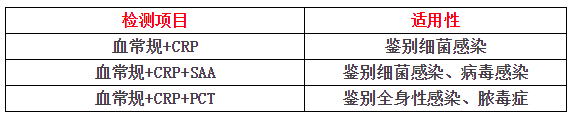
感染性疾病是临床常见病、多发病,若不能早期诊断并及时治疗,病情进展可导致脓毒症和多器官功能障碍综合征(MODS),甚至危及生命。感染早期的临床征象常不典型,如何选择高灵敏性、高特异性的的实验室诊断标志物,协助临床医生早期诊断对患者的病情做出快速、准确的诊断具有重要意义。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#PCT#
70
#感染性#
61
SAA以前不了解.学习了.
80
#CRP#
50
好文献学习了
91
好文献学习了
94
学习了受益匪浅
105