Future Oncol:帕洛诺司琼对高剂量化疗患者能有效的止吐
2015-02-28 范伟 MedSci原创
目的:间隔的帕洛诺司琼给药方案对多天大剂量化疗(HDC)的患者控制呕吐的疗效调查。 病人&方法: 58例病人每隔一天接受帕洛诺司琼静脉注射(iv)(0.25毫克)加上每日地塞米松(8毫克静脉注射,每天两次)的剂量。主要疗效终点是在整个急性期(直到化疗完成后的24小时)的完全控制(没有呕吐;没有使用救急止吐药,以及无轻微的恶心)。 结果:接受帕洛诺司琼和昂丹司琼的患者在急性期得到完全控制
目的:间隔的帕洛诺司琼给药方案对多天大剂量化疗(HDC)的患者控制呕吐的疗效调查。
病人&方法: 58例病人每隔一天接受帕洛诺司琼静脉注射(iv)(0.25毫克)加上每日地塞米松(8毫克静脉注射,每天两次)的剂量。主要疗效终点是在整个急性期(直到化疗完成后的24小时)的完全控制(没有呕吐;没有使用救急止吐药,以及无轻微的恶心)。
结果:接受帕洛诺司琼和昂丹司琼的患者在急性期得到完全控制的比例分别为81%和50%。帕洛诺司琼(优势比[OR]:4.37;p = 0.001)和更长持续时间的高剂量化疗方案(OR:3.47;p = 0.011)独立预测了更好的止吐效果。
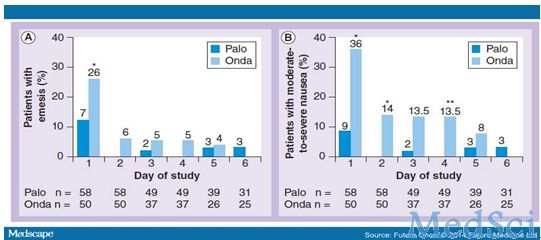
在每天的化疗方案治疗组中患者出现呕吐(A)或严重恶心(B)的比例。由于使用不同的方案,每个治疗组样本的大小递减。* p < 0.005 vs昂丹司琼方案(two-sided Fisher's exact test);
* * p < 0.05 vs昂丹司琼方案。缩写 Onda:昂丹司琼;Palo:帕洛诺司琼

在每天的化疗方案治疗组中需要药物救急的患者比例。由于使用不同的方案,每个治疗组样本的大小递减。* p < 0.005 vs昂丹司琼方案(two-sided Fisher's exact test);* * p < 0.05 vs昂丹司琼方案。缩写 Onda:昂丹司琼;Palo:帕洛诺司琼
结论:帕洛诺司琼每隔一天剂量加每天剂量的地塞米松对接受高剂量化疗的患者具有有效的止吐覆盖率。
原始出处
Aurora Mirabile, Luigi Celio, Michele Magni, Erminio Bonizzoni, Alessandro Massimo Gianni, Massimo Di NicolaDisclosures.Evaluation of an Every-other-day Palonosetron Schedule to Control Emesis in Multiple-day High-dose Chemotherapy.Future Oncol. 2014;10(16):2569-2578.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







总结的很好,学习了
98
#高剂量#
53
#帕洛诺司琼#
63
#Oncol#
68
很不错学习了
159
赞
144
赞
124
又多一个品种,接下来应该做头对头研究了,或做PCT,比较一下各种止吐药效果
144
不错!
96
赞!
121