Cell Metab:揭秘梦中杀手!科学家首次揭示动脉粥样硬化偏爱在凌晨形成的原因
2018-07-08 奇点糕 奇点网
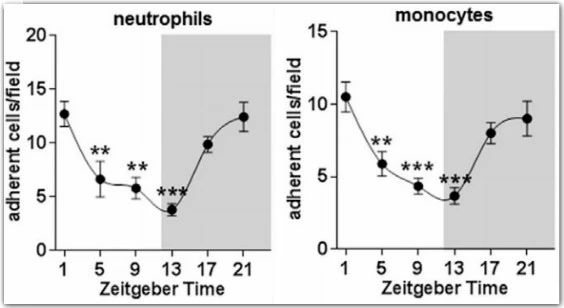
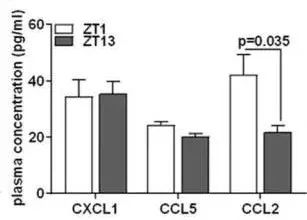
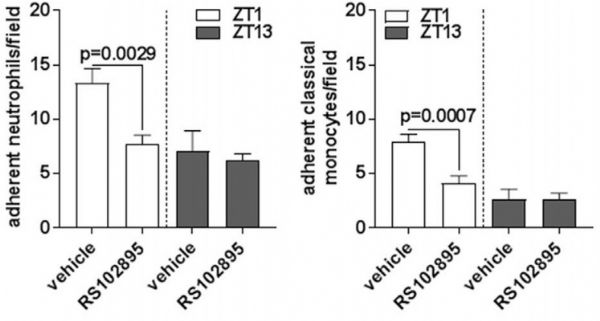
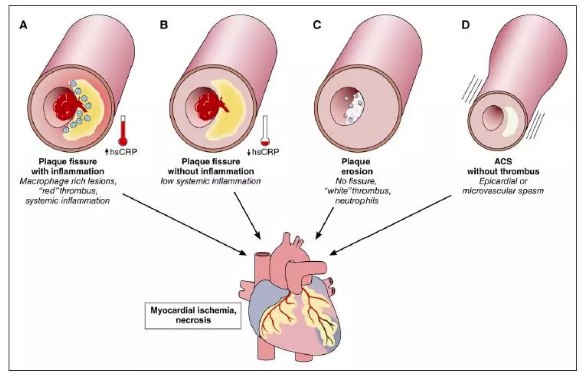
关于动脉粥样硬化的机制有多种学说,其中最受研究人员支持的当属“内皮损伤学说”。这个学说认为,氧化的低密度脂蛋白胆固醇堆积在动脉内壁上,造成了功能性损伤。为了应对损伤,免疫系统派出白细胞向伤口处集合。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
56
#粥样硬化#
56
#MET#
59
#Meta#
55
#Cell#
50
总以为想当然.结果人家发高分
85
谢谢分享学习
92
疾病第一大杀手.动脉粥样硬化正是冠心病等缺血性心血管疾病的的主要病理基础.结果:心.脑血管病高发病率.卒中.心梗.死亡率迅速增加.癌症低龄化显著.传统癌症患病率下降.结论:健康的生活方式显著变化降低.成为了第二大杀手.总之减少冲突.降低死亡率仍是医疗的目标.学习了.知行合一.--
82
学习谢谢分享
76
学习了
75