CSA&TISC2019丨卵圆孔未闭和隐源性卒中的谜团解疑
2019-06-30 国际循环编辑部 国际循环
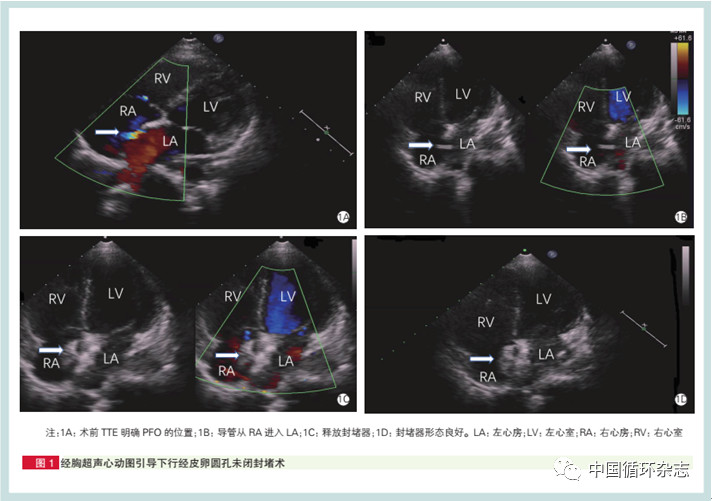
编者按:卵圆孔未闭(PFO)是一种常见的先天性心脏病,可通过反常性栓塞引起隐源性卒中(CS)。长期以来封堵治疗和药物治疗在预防CS复发方面一直存在争议,究竟哪一种治疗更优,PFO与CS存在怎样的关系?这均是亟待解决的问题。CSA&TISC 2019大会期间,中山大学附属第一医院范玉华教授在相关研究证据的基础上,详细解答了PFO与CS的关系,并指出很多待探讨的问题。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#隐源性卒中#
88
#TISC#
66
#ISC#
72
666
120
好
109
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
79
666
92