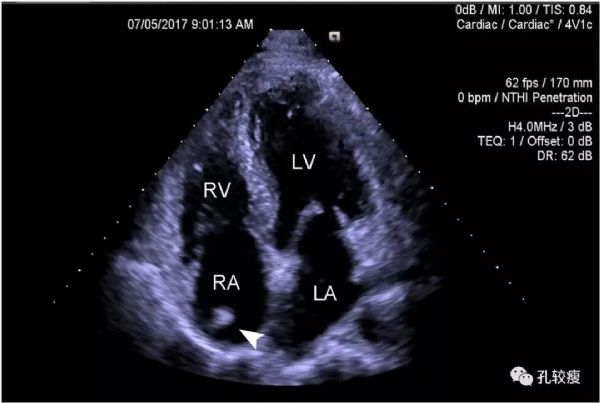
哪些心脏超声表现,几乎没有临床意义?
2019-10-11 孔令秋 孔较瘦
我们在临床中经常会遇到各种各样的问题,尤其是不从事心血管的医生以及患者和家属,他们对于一些心脏超声表现中的所谓「异常」,经常忧心忡忡,我们总要花费很大的气力去解释。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













好文,期待更多类似文章!
98
学习了
105
有点意思
135
#超声表现#
92
牛逼
131
#心脏超声#
101