BMC Cancer:评估每周低剂量贝伐珠单抗联合方案治疗铂耐药卵巢癌患者的疗效
2022-02-18 yd2015 MedSci原创
研究表明,每周低剂量贝伐珠单抗联合治疗较每月高剂量贝伐珠单抗改善铂耐药卵巢癌患者预后,今后需进一步验证。
贝伐珠单抗常用于卵巢癌患者的治疗。近期,日本团队在BMC Cancer杂志上发表了一项研究结果,目的是评估每周低剂量贝伐珠单抗与每月高剂量贝伐珠单抗治疗铂耐药卵巢癌患者的疗效。

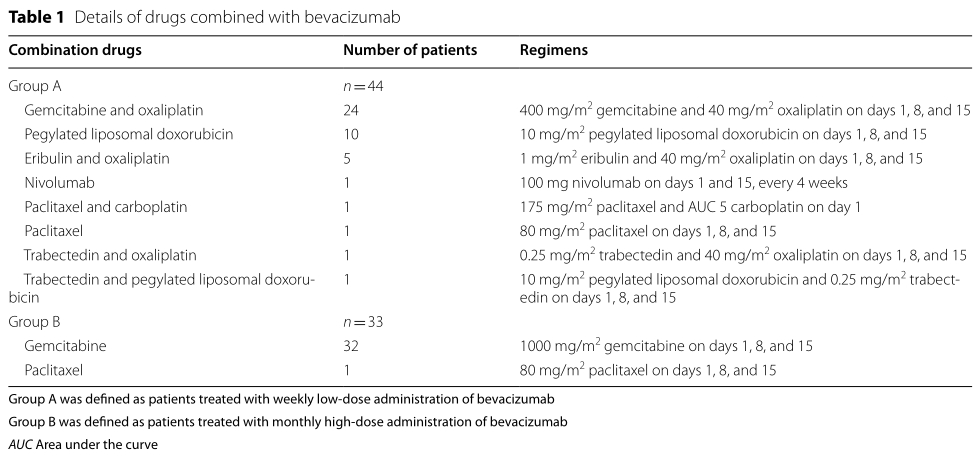
研究回顾性纳入两家医院使用贝伐珠单抗治疗的患者,A组患者为使用每周低剂量贝伐珠单抗(100mg d1和d8, 200mg d15)治疗,B组患者为使用每月高剂量贝伐珠单抗(15 mg/kg,d1)治疗。比较两组的疗效。
研究纳入A组44例,B组33例。两组的最佳应答,应答率以及临床获益率没有统计学差异,但是A组的持续缓解时间较B组明显延长,分别为8 (0–37)个月和5 (0–10)个月,有统计学差异(p < 0.01)。
A组患者的中位PFS优于B组(p<0.01);但是,两者的中位OS没有统计学差异( p = 0.58)。

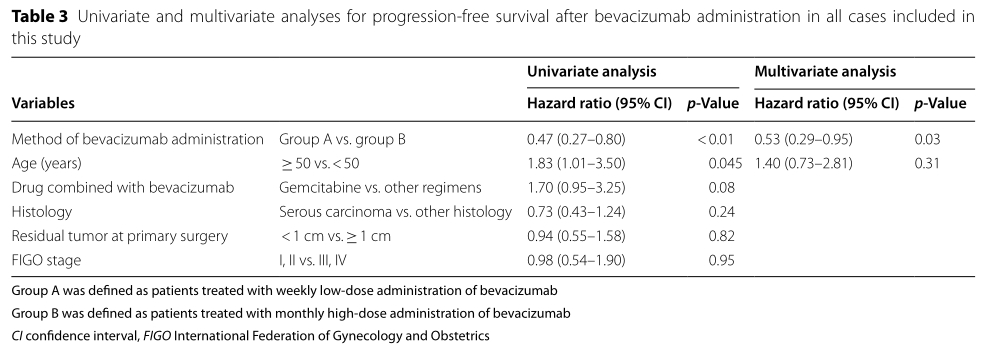
在PFS的多因素分析中,每周低剂量贝伐珠单抗治疗是PFS独立预后良好因素(HR=0.53,95%CI 0.29–0.95,p=0.03)。
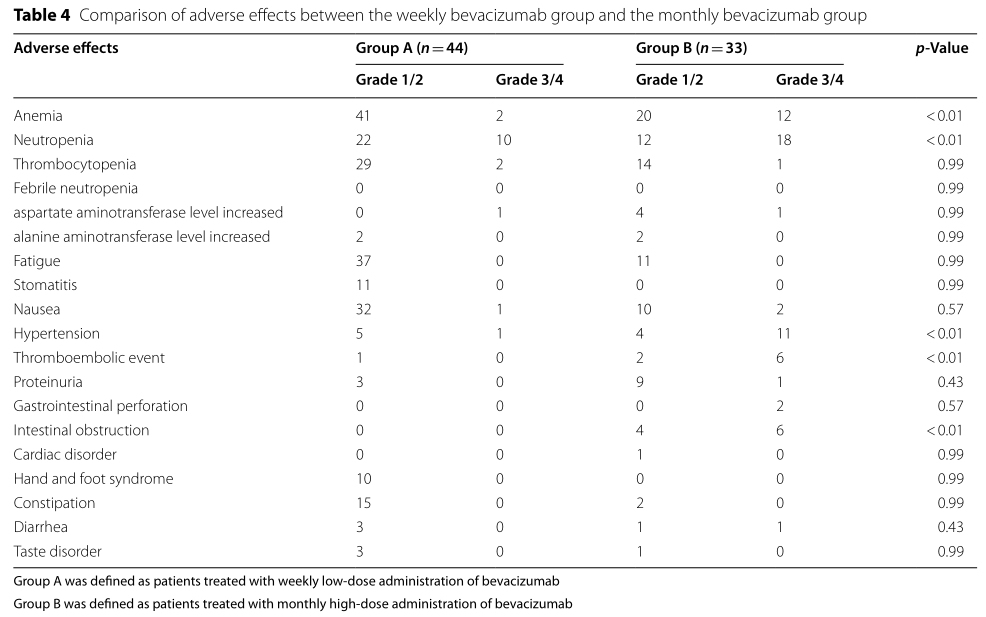
A组患者出现3/4级贫血(p<0.01),3/4级中性粒细胞减少(p<0.01), 3/4级高血压(p<0.01)、肠梗阻(p<0.01)和血栓栓塞事件(p<0.01)较B组明显减少。A组中,使用吉西他滨+奥沙利铂,聚乙二醇脂质体阿霉素和其他方案治疗患者在PFS(分别为6, 12, 和5个月,p < 0.12),应答率(分别为20%, 30%, 和10%, p = 0.55), 临床获益率 (分别为75%, 100%,和80%,p = 0.32), 和持续应答时间(分别为4, 9.5,和3个月; p < 0.13) 等方面没有统计学差异。
综上,研究表明,每周低剂量贝伐珠单抗联合治疗较每月高剂量贝伐珠单抗改善铂耐药卵巢癌患者预后,今后需进一步验证。
原始出处:
Suminokura J, Miyamoto M, Yoshikawa T, Kouta H, Kikuchi Y, Hada T, Ishibashi H, Ito T, Iwahashi H, Kakimoto S, Suzuki R, Matsuura H, Kishimoto N, Takano M. Potential efficacy of weekly low-dose administration of bevacizumab as a combination therapy for platinum-resistant ovarian carcinoma: a retrospective analysis. BMC Cancer. 2022 Feb 16;22(1):176. doi: 10.1186/s12885-022-09271-3. PMID: 35172766.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#铂#
124
#BMC#
70
#联合方案#
54
#贝伐单抗#
0
#贝伐珠#
56
#贝伐#
90
#低剂量#
69
提供了一个新思路
74