JCLA:ELISA和斑点印迹法检测Graves病TSH受体抗体的比较
2022-03-04 从医路漫漫 MedSci原创
Graves病(Graves‘s disease,GD)是一种自身免疫性疾病,约占总人口的0.5%,女性发病率高于男性。
背景:Graves病(Graves‘s disease,GD)是一种自身免疫性疾病,约占总人口的0.5%,女性发病率高于男性。临床上,GD以促甲状腺激素(TSH)水平抑制、甲状腺激素过度刺激和抗甲状腺抗体产生为特征。目前公认促甲状腺激素受体自身抗体(TRAb)是GD的血清学标志,通常有助于将GD与其他原因甲亢相鉴别。此外,TRAb的作用不仅在确认GD诊断方面,而且在预测GD的临床病程、复发风险和治疗反应方面也有潜力。是甲状腺功能亢进症(甲亢)的主要病因。抗促甲状腺激素受体/TSHR抗体(TRAb)与甲状腺功能亢进症(甲亢)有关,被认为是GD的诊断标记物。因此,我们研制了一种人TSHR-169重组蛋白(hTSHR-169),该重组蛋白可特异性识别GD患者血清中的TRAb,并比较了ELISA和斑点印迹检测TRAb对GD的诊断能力。
方法:从印尼人群中选取20例GD患者和20例健康人作为研究对象。定量测定TRAb浓度和密度。采用受试者-操作曲线(ROC)分析进行对比分析。
结果:斑点印迹法检测TRAb的最低浓度为100 ng,抗血清稀释度为1:60。与斑点印迹法相比,ELISA法诊断GD的AUC更高(分别为0.95和0.85)。使用推荐的临界值,通过比较两种检测方法对临床诊断的特异性和敏感性来检验这两种检测方法的效率。ELISA检测的敏感性和特异性分别为80%和95%,斑点印迹检测的敏感性和特异性分别为70%和95%。

图1 HTSHR-169在pET28a(+)载体中的F I G U R E 1克隆。(A)编码hTSHR-169蛋白的pET28a(+)表达载体的示意图。(B)重组克隆的PCR产物(扩增片段大小689bp);M:DNA标记;NC,阴性对照;泳道1-5:重组克隆,复制1-5。(C)重组pET28a-hTSHR-169表达载体的限制性内切酶分析。M:DNA标记;泳道1:未消失的pET28a(+)载体;泳道2:酶切的pET28a(+)载体;泳道3:未酶切的重组pET28a(+)载体;泳道4:带有BamHI和XhoI的酶切重组pET28a(+)载体,其中5.32kb是指pET28a(+)载体的片段(箭头),411bp的条带是指hTSHR-169的cDNA插入片段(箭头)。(D)针对hTSHR序列的cDNA插入序列之间的比对

图2 (A)0.1 mM IPTG诱导hTSHR-169融合蛋白的表达谱。样品用12%SDS-PAGE凝胶分离。考马斯亮蓝染色可见蛋白条带。M:蛋白标记物;NI:不含IPTG;I:含IPTG。(B)Western blot检测纯化的hTSHR-169融合蛋白的抗原性。纯化的hTSHR-169片段与抗TSHR单克隆抗体和GD患者血清共同孵育时,可检测到预期大小为16.8 kDa的单一条带,而健康对照则无此条带。M:蛋白质标记物。(C)优化斑点杂交方法,将重组hTSHR-169斑点于NCM上(不同浓度10-1000 ng),并与GD患者或健康人血清(2倍稀释度1:20~1:120)孵育。Ag(−)或Ab(−)分别表明只能用重组TSHR-169或TRAb探测NCM。箭头表示与对照相比,检测GD样品中TRAB所需的最低浓度

图3 (A)20个已知GD和对照样本的免疫反应性。每个样本均为一式两份;Ag(−)或Ab(−)分别表示仅用重组TSHR-169或TRAb探针的NCM。(B)用酶联免疫吸附试验(ELISA)测定GD和对照样本中的TRAb水平。(C)斑点印迹法检测TRAb密度。(D)以20例GD患者为疾病变量,20例正常人为对照变量,比较TRAb-ELISA和斑点印迹分析ROC结果。GD,Graves病;HC,健康对照
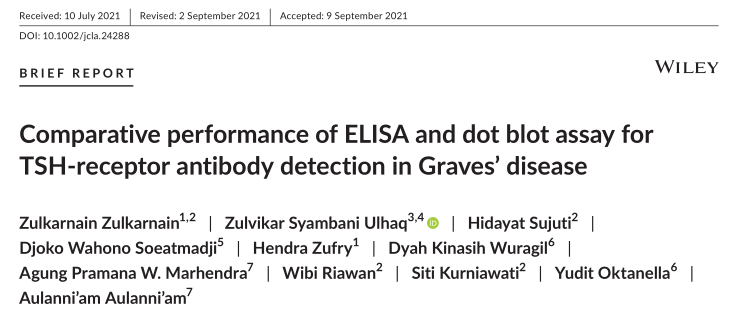
表1 ELISA与斑点印迹法检测TRAb的比较
结论:虽然斑点印迹法的检测效果低于ELISA法,但斑点印迹法是一种简便、快速的诊断方法,适用于医疗机构有时难以进入的农村地区的GD诊断。
原文出处:Zulkarnain Z, Ulhaq ZS, Sujuti H, et al.Comparative performance of ELISA and dot blot assay for TSH-receptor antibody detection in Graves' disease.J Clin Lab Anal 2022 Feb 20
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Graves#
73
好
86
#TSH#
90
#Graves病#
80