病例:肺真菌感染切忌误诊
2018-04-12 MedSci MedSci原创
肺部真菌感染是由真菌感染引起的支气管-肺部疾病,包括原发性和继发性肺部真菌感染。肺真菌感染临床表现常无特异性,故容易误诊。以下就是一例误诊案例。 该患者为一个41岁男性。1个月前患者发现颈部、颌下及腋窝出现数个增大的淋巴结,其中颌下淋巴结有压痛。同时左胸部出现疼痛,按压时疼痛明显,但无放射痛,偶伴非刺激性咳嗽,无发热、头痛,无咳痰、咯血,口服头孢克洛治疗1周无效。在当地医院对下颌淋巴结穿

肺部真菌感染是由真菌感染引起的支气管-肺部疾病,包括原发性和继发性肺部真菌感染。肺真菌感染临床表现常无特异性,故容易误诊。以下就是一例误诊案例。
该患者为一个41岁男性。1个月前患者发现颈部、颌下及腋窝出现数个增大的淋巴结,其中颌下淋巴结有压痛。同时左胸部出现疼痛,按压时疼痛明显,但无放射痛,偶伴非刺激性咳嗽,无发热、头痛,无咳痰、咯血,口服头孢克洛治疗1周无效。在当地医院对下颌淋巴结穿刺活检显示小淋巴细胞,多见未分化细胞,未见肿瘤细胞。为明确诊断,7天前转来我院就诊。门诊查前胸部X 线片检查发现左下肺野结节影;胸部CT 检查显示左侧胸膜增厚、粘连,胸膜下结节;PET-CT 显示左下肺结节及全身多发淋巴结代谢异常增高,考虑恶性病变可能。拟“左肺下叶结节”收入我科。
患者既往体健,有海鲜过敏史。否认养鸽子和接触禽类史。久居湖北,吸烟16 年,无饮酒嗜好。体格检查:一般情况良好,全身浅表淋巴结增大,质韧,活动好,大小不一,部分淋巴结有触痛。心、肺、腹、神经系统及皮肤科检查未见明显异常。
为了明确诊断,入院完善实验室检查:血常规、血生化全项及凝血功能筛查未见异常;HIV检查阴性;甲状腺功能正常;肿瘤标志物包括癌胚抗原、CA19-9、鳞状细胞癌相关抗原、细胞角蛋白19片段、神经元特异性烯醇酶、组织多肽抗原及胃泌素释放肽前体未见异常。
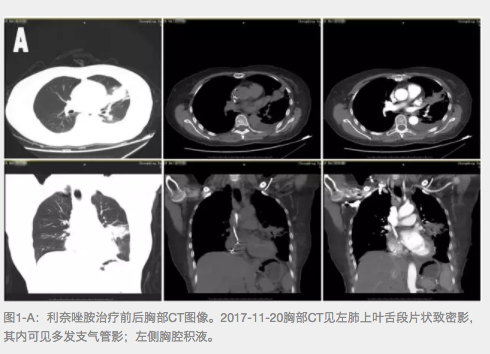
复查影像学检查:胸部X 线片显示左下肺野一小结节阴影、斑点状影。胸部CT 显示左侧胸膜下结节、扁平状高密度影,左下斜裂见条片状影。PETCT显示左下肺后基底段一1.1 cm × 0.8 cm 结节影;左肺下舌段见少许结节及条片影;双侧颈部、腋窝、纵隔及右肺门区、腹腔内胃贲门旁、肝门区、胰头旁、腹膜后腹主动脉旁、髂血管旁及髂内外、腹股沟区均可见多发淋巴结影,结论:左下肺结节及全身多发淋巴结代谢异常增高,考虑恶性病变可能。
患者症状考虑肿瘤可能性,但无法明确诊断。需进一步确认。告知家属及患者病情后建议经胸腔镜行左肺下叶楔形切除术及左侧腋窝淋巴结活检术。
肺病变组织病理显示肺组织中见灶性小脓肿形成,伴周围大量多核巨细胞反应及上皮样组织细胞增生(图1a,1b)。
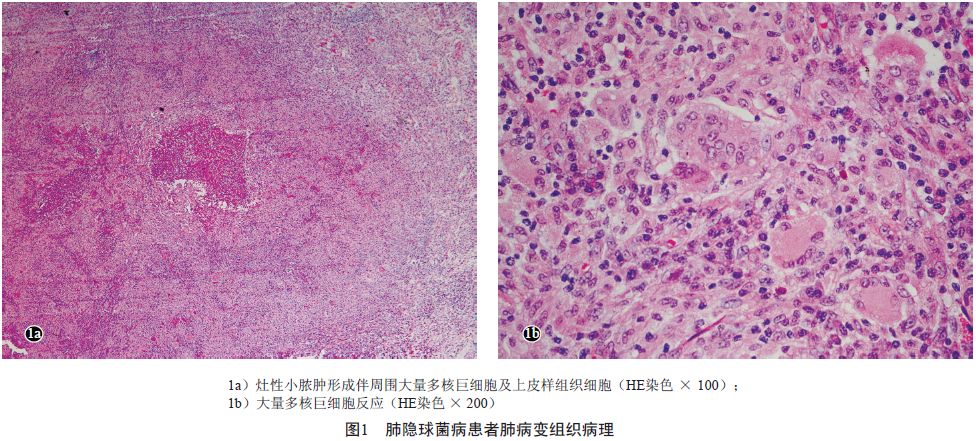
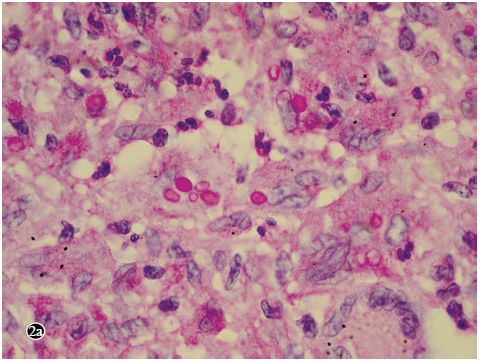
考虑为肉芽肿性炎。过碘酸- 雪夫染色(PAS)可见红色、多量、大小不一的圆形酵母细胞;抗酸染色阴性。腋窝淋巴结组织病理检查显示淋巴滤泡增生,生发中心明显扩大,其周围小血管增生、扩张并出血,符合反应性增生性改变。
患者组织病理提示为隐球菌感染,,即给予真菌相关的血清学试验,结果显示血清隐球菌荚膜多糖抗原乳胶凝集试验阴性;半乳糖甘露聚糖试验(GM试验)阴性;β-1,3-D- 葡聚糖试验(G 试验)阴性。对肺部病变组织切片行隐球菌免疫组化染色,结果阳性。

根据上述检查最终明确了“伴淋巴结增大的肺隐球菌病”的诊断。
后予以患者口服氟康唑450 mg/d 治疗3 个月,全身浅表淋巴结缓慢缩小,复查血清隐球菌荚膜多糖抗原乳胶凝集试验仍呈阴性。停药后随访1 年无复发。
讨论:
肺隐球菌病临床表现和影像学表现均无特异性,易误诊为普通肺炎、肺结核或肺部肿瘤。当怀疑肺隐球菌病时应尽快行血清隐球菌荚膜多糖抗原乳胶凝集试验、肺活检或手术病理和组织真菌培养[1]。血清隐球菌荚膜多糖抗原乳胶凝集试验和T 细胞斑点试验联合检测对肺结核并发肺隐球菌病具有诊断价值[2]。该例因全身浅表淋巴结增大而行胸部影像学检查,发现肺部有阴影,临床上亦考虑肺部肿瘤可能性大,因此,给予患者行左肺下叶楔形切除术及左侧腋窝淋巴结活检术。术后肺病变组织病理显示为肉芽肿炎改变,PAS 染色可见较多的酵母细胞,提示为肺隐球菌感染,而腋窝淋巴结组织病理检查显示反应性增生性改变。本例提示对于肺病变组织病理显示为肉芽肿炎改变的患者,手术医生应警惕真菌感染的可能,应对病变组织行真菌培养,以明确致病菌。由于本例患者未行肺病变组织真菌培养,因此,我们对肺病变组织病理切片进行了针对隐球菌的免疫组化染色,结果显示阳性,最后确诊为肺隐球菌病。
所有肺部及肺外隐球菌感染的患者应排除伴发中枢神经系统感染的可能,均建议行腰穿检查,但对肺部隐球菌感染无症状、非弥漫性病变的免疫正常宿主,且血清隐球菌抗原阴性或低滴度者除外[3]。因剖胸探查或误诊为肿瘤或其他病变行病灶手术切除者,建议术后常规应用抗真菌药物治疗至少2 个月[3]。本例患者病灶已行手术切除,因此,给予患者口服氟康唑450 mg/d 治疗3 个月,全身增大的浅表淋巴结逐渐缩小,复查血清隐球菌荚膜多糖抗原乳胶凝集试验仍阴性,遂停药,随访1 年未见复发。该例比较特殊之处是同时出现全身淋巴结增大,经过2 次淋巴结组织病理检查证实是反应性增生性改变,且肺部病变组织病理显示有大量多核巨细胞反应,血清隐球菌荚膜多糖抗原乳胶凝集试验阴性。提示隐球菌可能经肺部侵犯该患者后,由于患者免疫功能正常,全身淋巴结增大是对隐球菌病原体的抵抗,这样将隐球菌病原体导致的病变局限于肺部,阻止了隐球菌荚膜多糖抗原进入血液等器官,因此,该例患者血清隐球菌荚膜多糖抗原乳胶凝集试验阴性。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#真菌#
63
#真菌感染#
67
学习学习学习
102
学习了
91
学习学习了
101
学习学习学习
79
治疗3个月.多久用药起效?
84
如果能够有影像学资料就更好了
44
学习了
53
学习
56