Hepatology:早期诊断肝癌的新型分子标记!
2017-10-24 MedSci MedSci原创
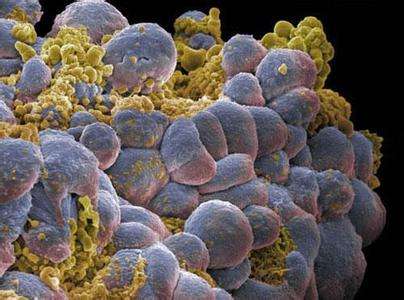
由于肝细胞癌(HCC)的早期检测可以显着提高存活率,因此,早期诊断HCC的精准方法在临床十分重要。近期,一项发表在杂志Hepatology上的研究旨在调查在癌前病变中可能检测到的HCC早期进展的分子标记。研究者们设计了基因选择策略,通过对人类不同分期HCC组织的转录组和临床病理资料的综合分析,包括癌前病变、低级别和高级别发育不良结节来鉴定潜在的驱动因子。通过检测HCC和癌前病变中所选择的分子来指导
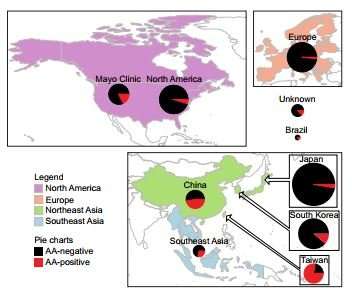
由于肝细胞癌(HCC)的早期检测可以显着提高存活率,因此,早期诊断HCC的精准方法在临床十分重要。近期,一项发表在杂志Hepatology上的研究旨在调查在癌前病变中可能检测到的HCC早期进展的分子标记。研究者们设计了基因选择策略,通过对人类不同分期HCC组织的转录组和临床病理资料的综合分析,包括癌前病变、低级别和高级别发育不良结节来鉴定潜在的驱动因子。通过检测HCC和癌前病变中所选择的分子来指导基因选择过程。最终,研究者们选择了10个基因元件作为候选物,通过免疫组织化学染色显示,并与目前流行的三重HCC诊断标记:磷脂酰肌醇蛋白聚糖3,谷氨酰胺合成酶和热休克蛋白70相比,BANF1、PLOD3和SF3B4是HCC的决定标记,在HCC患者中,它们具有较好的早期诊断能力。此外,靶向灭活BANF1、PLOD3和SF3B4可以通过选择性调节EMT和细胞周期蛋白来抑制体外和体内肝肿瘤的发生。使用含有三种基因的siRNA的纳米颗粒的处理抑制了自发性小鼠HCC模型中的肝肿瘤发生率和肿瘤生长速度。此外研究还证明,SF3B4过表达触发SF3b复合物将肿瘤抑制因子KLF4转录物剪接到非功能性跳过的外显子转
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#早期诊断#
66
#EPA#
68
学习学习.了解了解
85
谢谢分享谢谢分享
77