Eur J Cancer:单纯前哨淋巴结切除有望替代早期宫颈癌的盆腔淋巴结清扫!
2021-03-29 MedSci原创 MedSci原创
近年来,前哨淋巴结(SN)识别被认为是评估淋巴管转移的有效方法
早期宫颈癌最重要的预后因素是淋巴结状态。盆腔淋巴结清扫已成为早期宫颈癌患者的标准手术方式。近年来,前哨淋巴结(SN)识别被认为是评估淋巴管转移的有效方法,可以提高转移性疾病的检出率,但就降低复发率而言,省略盆腔淋巴结清扫的好处尚未得到证实。
近日,《欧洲癌症杂志》上发表的一项研究“Sentinel lymph node biopsy and morbidity outcomes in early cervical cancer: Results of a multicentre randomised trial (SENTICOL-2)”,评估了省略盆腔淋巴结清扫和早期宫颈癌预后的相关性。
这是一项开放式研究,将早期宫颈癌患者(FIGO 2009分期IA2~IIA1)随机分为单纯SN切除组(SN组)或SN+盆腔淋巴结清扫组(SN+PLND组)。所有患者都接受了肿瘤根治性手术。主要终点是与淋巴结清扫相关的发病率;次要终点是3年无复发生存率。
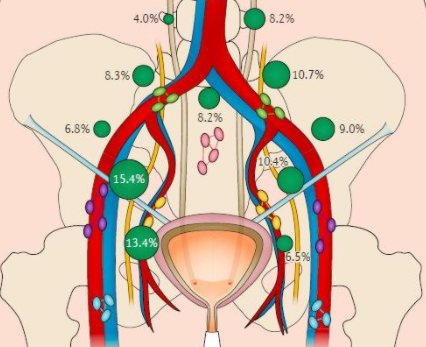
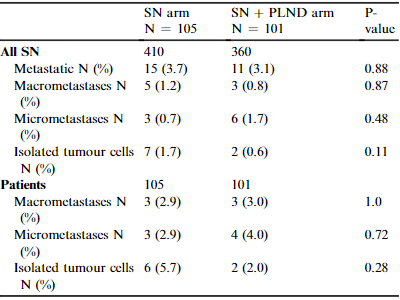
两组的转移性SN病例
共招募了206例患者,随机分至SN组(105例)和SN+PLND组(101例)。大多数患者为IB1期病变(87.4%)。SN+PLND组无假阴性病例。
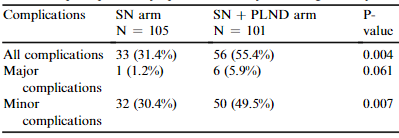
术后6个月内的淋巴管发病率
SN组淋巴管发病率(31.4%)明显低于SN+PLND组(51.5%;p=0.0046),SN组的术后神经症状发生率也明显低于SN+PLND组(7.8% vs 20.6%,p=0.01)。然而,两组患者发生明显淋巴水肿的比例并无显著差异。
三年无复发存活率
在术后6个月,两组淋巴结发病率的差异随着时间的推移而降低。SN组和SN+PLND组的3年无复发生存率分别为92.0%和94.4%,差异无统计学意义。
综上,在早期宫颈癌中,与SN+PLND相比,单纯SN切除(即省略盆腔淋巴结清扫)与早期淋巴管发病率降低有关,且未明显影响患者的无复发生存率。
原始出处:
Mathevet Patrice,Lécuru Fabrice,Uzan Catherine et al. Sentinel lymph node biopsy and morbidity outcomes in early cervical cancer: Results of a multicentre randomised trial (SENTICOL-2).[J] .Eur J Cancer, 2021, 148: 307-315.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















很好的学习,期待更多的数据报告。
68
#淋巴结清扫#
70
#淋巴结#
53
#宫颈#
57
#前哨淋巴结#
0
有望,但是依靠早起筛查
90