JACC:明显增加不良事件风险!主动脉夹层或动脉瘤患者应避免使用氟喹诺酮类药物
2021-04-20 MedSci原创 MedSci原创
主动脉夹层或动脉瘤患者应避免使用氟喹诺酮类药物
近期,基于人群的研究表明,使用氟喹诺酮类(FQ)药物与主动脉夹层(AD)和动脉瘤(AA)的风险增加有关。但是,尚无证据表明FQ是否会增加确诊为AD或AA的患者的不良事件风险。
本研究旨在明确FQ的使用是否会增加高风险人群(AD和AA患者)的动脉瘤相关不良事件和死亡的风险。
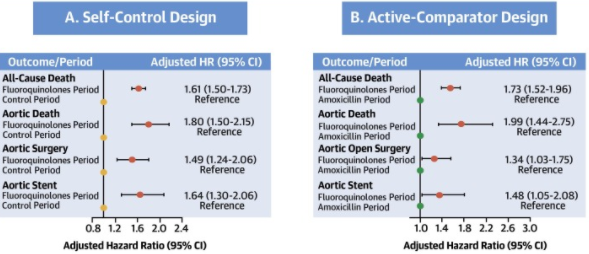
这是一项采用台湾国民健康保险研究数据库数据进行的一项回顾性队列研究。共确定了31570位在2001-2013年确诊AD或AA后存活的成年患者。随访过程中,研究人员将每位患者的每年分成了6个数据单元(2个月为一时间单元)。每两个月评估一次协变量和风险暴露(FQ)。此外,研究人员还使用了另一种常见的抗生素阿莫西林作为阴性对照。
FQ暴露与AD或AA患者预后的相关性
总体上,FQ暴露与AD或AA患者的全因死亡风险(校正风险比 1.61,95% CI 1.50-1.73)、主动脉死亡(1.80,95% CI 1.50-2.15)以及后续进行主动脉手术的风险更高相关。
阿莫西林暴露与上述任何结局的风险均无显著相关性。此外,亚组分析表明,FQ的效应在AD和AA组患者之间无明显差异。
总之,与阿莫西林暴露相比,AD或AA患者采用氟喹诺酮类药物治疗与不良结局预后的风险更高相关。因此,这类高风险患者应避免使用FQ治疗,除非没有其他可用的药物。
原始出处:
Chen Shao-Wei,Chan Yi-Hsin,Chien-Chia Wu Victor et al. Effects of Fluoroquinolones on Outcomes of Patients With Aortic Dissection or Aneurysm. J Am Coll Cardiol, 2021, 77: 1875-1887. https://doi.org/10.1016/j.jacc.2021.02.047
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#氟喹诺酮类药物#
96
#喹诺酮#
95
#不良事件风险#
70
#JACC#
60
#ACC#
55
#主动脉#
59
#动脉夹层#
67
#氟喹诺酮#
77
很棒
95
与阿莫西林暴露相比,AD或AA患者采用氟喹诺酮类药物治疗与不良结局预后的风险更高相关。因此,这类高风险患者应避免使用FQ治疗,除非没有其他可用的药物。
95