Blood:母细胞性浆细胞样树突状细胞肿瘤
2019-07-03 MedSci MedSci原创
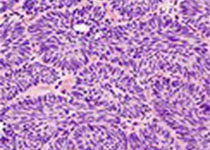
母细胞性浆细胞样树突状细胞肿瘤(Blastic plasmacytoid dendritic cell neoplasm, BPDCN)是一种不常见的血液恶性肿瘤,预后差。BPDCN临床表现的相关数据有限,因为现有报道的结果主要来自小规模的回顾性研究,缺乏标准化的治疗指南。
中心点:
现代多中心BPDCN人群的预后为靶向治疗提供了一个基准。
60岁以下、核型正常和TdT阳性患者预后相对较好,普拉曲沙和Enasidenib对BPDCN具有一定治疗活性。
摘要:
母细胞性浆细胞样树突状细胞肿瘤(Blastic plasmacytoid dendritic cell neoplasm, BPDCN)是一种不常见的血液恶性肿瘤,预后差。BPDCN临床表现的相关数据有限,因为现有报道的结果主要来自小规模的回顾性研究,缺乏标准化的治疗指南。
最近,IL-3细胞毒素结合物Tagraxofusp获得美国食品和药物管理局(FDA)批准进行1/2期试验,这是首次获批进行治疗BPDCN的试验。但由于目前在这项或任何临床研究中,还没有匹配的内部比较器,BPDCN试验检测新药物的结果很难与替代疗法进行比较。因此Justin Taylor等人尝试在tagraxofusp问世之前,定义一组BPDCN患者的临床特征和预后。
在59个关于BPDCN患者的研究中,从确诊起的总体存活期中位值为24个月,预后与“仅皮肤”表现或伴有全身性疾病的患者相似。一线强化治疗和“淋巴样”化疗方案可改善患者预后。
仅有55%的患者进行了强化化疗,42%的患者进行了干细胞移植。确诊时与预后不良相关的临床特征有60岁以上、核型异常和BPDCN细胞的TdT阴性。此外,研究人员还确定了部分患者对普拉曲沙和Enasidenib治疗的疾病反应。
总而言之,本研究强调了现代BPDCN患者的不良预后以及对新治疗方法的需求。正在进行的BPDCN临床试验的结果可以相对地对当下的队列进行评估。
原始出处:
Justin Taylor, et al.Multicenter Analysis of Outcomes in Blastic Plasmacytoid Dendritic Cell Neoplasm Offers a Pre-Targeted Therapy Benchmark.Blood 2019 :blood.2019001144; doi: https://doi.org/10.1182/blood.2019001144
本文系梅斯医学(MedSci)原创编译,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#细胞性#
71
#浆细胞样树突状细胞#
85
#浆细胞样#
82
#浆细胞#
71
谢谢了,学习
131