Cell:CAR-T之父全新Cell论文:发现新靶点,助力CAR-T攻克实体瘤
2021-12-06 “ E药世界”公众号 “ E药世界”公众号
癌症免疫疗法的兴起为广大癌症患者带来了新的希望。其中,CAR-T细胞疗法已被证明是对抗血液类癌症的强大武器,但它们对抗实体瘤的效果要差得多,部分原因是一种被称为T细胞衰竭的过程。然而,在很大程度上,科
癌症免疫疗法的兴起为广大癌症患者带来了新的希望。其中,CAR-T细胞疗法已被证明是对抗血液类癌症的强大武器,但它们对抗实体瘤的效果要差得多,部分原因是一种被称为T细胞衰竭的过程。然而,在很大程度上,科学家们对T细胞衰竭过程的认知还不够,更多的分子细节仍有待进一步的阐明。
近日,美国宾夕法尼亚医学院 Carl June 团队在国际顶尖学术期刊 Cell 上发表题为:An NK-like CAR T cell transition in CAR T cell dysfunction 的研究论文。
这项研究基于一个新的研究模型全面解析用于攻击胰腺肿瘤的CAR-T细胞的衰竭过程,他们观察到,模型中的CAR-T细胞衰竭过程与患者的T细胞非常相似。该模型还发现两种遗传调节因子——ID3和SOX4,在T细胞衰竭过程中发挥着重要作用,将它们沉默后将延长CAR-T细胞的效应时间。
CAR-T细胞,是将来自患者血液的天然抗感染和抗癌的免疫细胞T细胞在体外进行基因重编程,这种重编程改变了患者的T细胞,使之能够识别患者体内癌细胞上的抗原标记物。随后,再利用细胞培养技术扩增这些CAR-T细胞,并将其重新注入患者体内以攻击癌症。
自2017年以来,CAR-T技术已被美国FDA批准用于治疗某些淋巴瘤和白血病。令人兴奋的是,在许多情况下,CAR-T细胞在这些癌症处于晚期时也有良好的治疗效果,甚至完全治愈了癌症患者。
然而,当T细胞暴露在目标抗原下的时间过长时(大约几周),就会引发T细胞衰竭。也正由于T细胞衰竭现象的存在,CAR-T细胞对实体肿瘤形成的癌症没有那么有效,这种现象被认为是一种进化上的机制,可以防止这些强大的免疫细胞对身体造成过多的附带损害。
CAR-T细胞功在接受抗原刺激过程中逐渐出现衰竭现象
在这项新研究中,研究人员在实验室环境下开发了一个T细胞衰竭模型,以便更深入地研究它,希望找到逆转它的方法。他们将CAR-T细胞与一种叫做间皮素的细胞标记物(在胰腺和其他一些肿瘤的表面发现)结合,并将T细胞与表达间皮素的胰腺肿瘤细胞接触,持续四周。
在T细胞衰竭模型中,CAR-T细胞转变为NK样细胞
T细胞的反应是表现出典型的衰竭迹象,但也有之前研究中不明显的迹象。这些新的衰竭现象包括一些T细胞的身份改变,这样它们部分地恢复成一种免疫细胞类型——NK细胞,它被认为是T细胞的远亲。
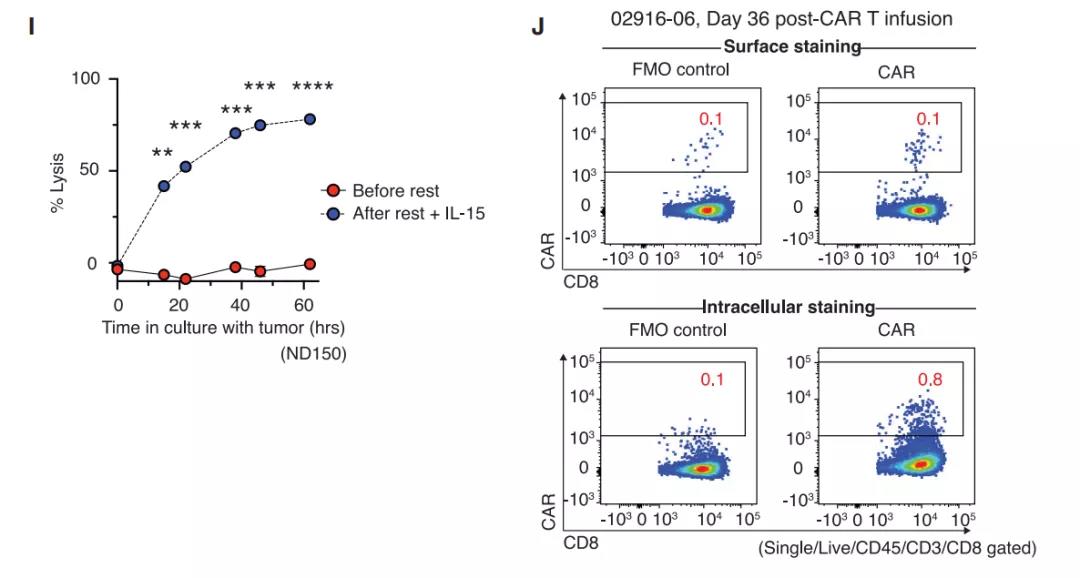
与之相印证,研究团队也在癌症患者体内耗尽的CAR-T细胞中发现了同样的T细胞向NK细胞转变的迹象。

功能障碍CAR-T细胞的转录动力学
更重要的是,研究小组还观察到CAR-T细胞的衰竭伴随着两种蛋白质的水平激增,即ID3和SOX4,它们是免疫细胞中大量基因的主开关。进一步研究显示,将ID3和SOX4这两个T细胞衰竭开关沉默之后,可以让CAR-T细胞在长时间暴露于肿瘤细胞后仍然保持其肿瘤杀伤效果。
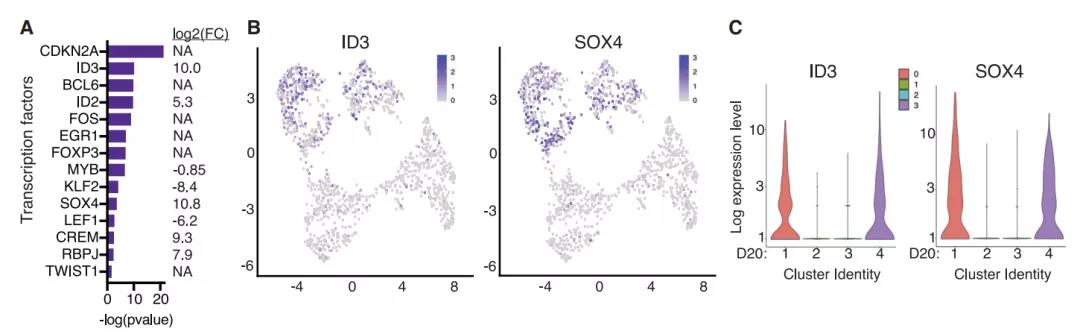
CAR-T细胞的衰竭伴随着ID3和SOX4表达量的激增
因此,这项研究指出了一种特定的策略,即抑制ID3和SOX4,这可能有助于CAR-T细胞更好地对抗实体肿瘤。
宾夕法尼亚大学细胞免疫疗法中心主任、本研究的通讯作者之一 Regina Young 博士说道:“这些发现令人兴奋,不仅在于它们从本质上验证了我们基于细胞模型探索,CAR-T细胞生物学和持续改进免疫治疗方面的效用,还在于它们具有潜在的临床意义,使癌症患者受益。”
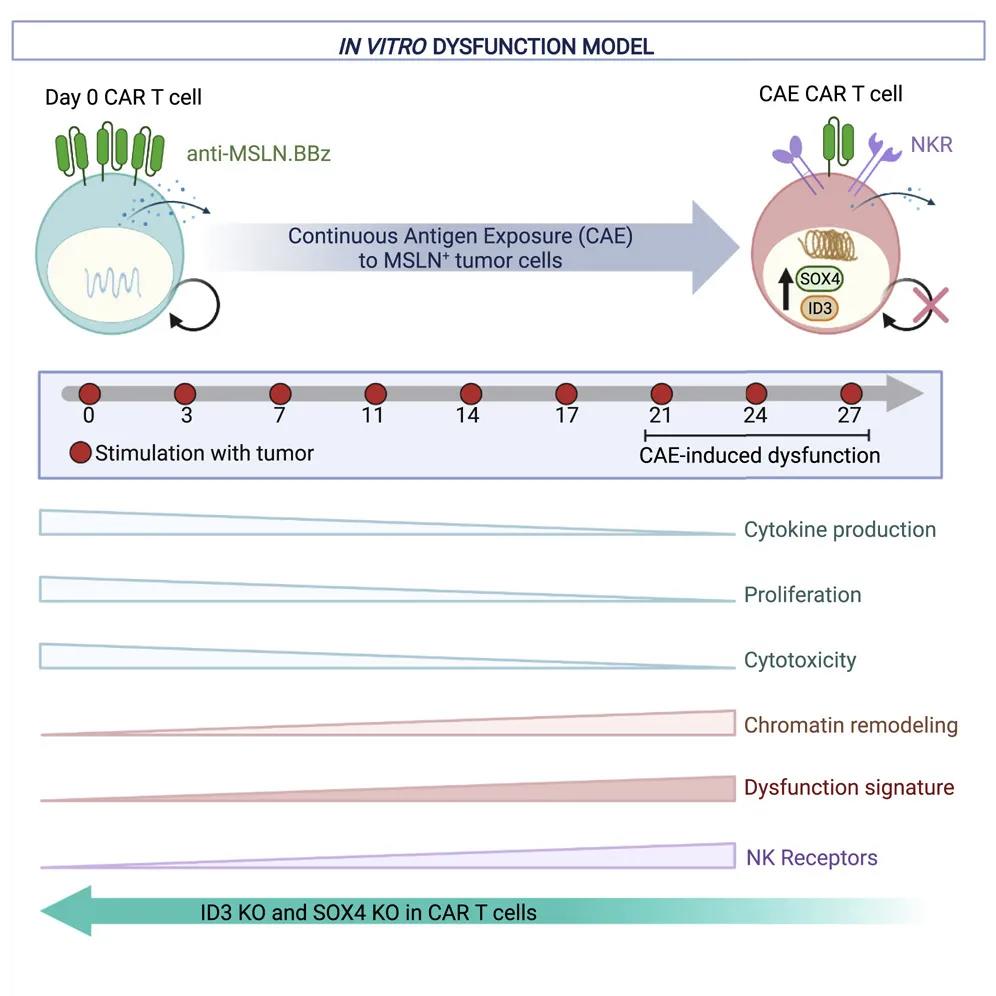
总的来说,这项发表于 Cell 的新研究表明,ID3和SOX4在T细胞衰竭中扮演着重要的角色,将其沉默敲除将指导下一代CAR-T细胞疗法的发展,更有效地对抗实体癌症!
原始出处:
Charly R. Good, et al. An NK-like CAR T cell transition in CAR T cell dysfunction. Cell, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
0
#Cell#
56
#CAR-#
67
#新靶点#
57
不断学习
108
上海市女医师协会从2021年9月启动
104