Neuromodulation:神经刺激对卒中后吞咽困难的影响的meta分析
2022-01-21 MedSci原创 MedSci原创
吞咽障碍(吞咽困难)是中风后常见的并发症,据报道发病率为37%至78%。吞咽困难的生理和心理社会后果是毁灭性的。它与营养不良、脱水、吸入性肺炎、住院时间延长和死亡率增加有关。患者在进餐期间经常经历焦虑
吞咽障碍(吞咽困难)是中风后常见的并发症,据报道发病率为37%至78%。吞咽困难的生理和心理社会后果是毁灭性的。它与营养不良、脱水、吸入性肺炎、住院时间延长和死亡率增加有关。患者在进餐期间经常经历焦虑、不适和尴尬,导致社交退缩和生活质量低下。吞咽困难可能在中风的前几周自行缓解,但超过50%的患者在出院时有持续性吞咽困难。卒中后吞咽困难相关的医疗费用很高,吞咽困难的持续存在会给卒中患者带来长期的经济和社会负担。中风后吞咽困难的治疗包括补偿策略,如改变饮食一致性、饮食姿势和喂养方法、吞咽肌肉组织的康复训练以建立力量和协调、针灸和物理感觉刺激,如触觉或热刺激。然而,这些疗法的疗效仍有争议。
由于缺乏有效的治疗方法,研究人员探索了通过增强神经可塑性促进康复的替代方案。吞咽由中枢神经系统调节,包括从大脑皮层到颅神经的结构。对麻醉和清醒动物的早期研究表明,双半球皮层控制吞咽肌肉组织。除了中枢或皮质神经刺激外,外周神经通路的刺激可能对卒中后吞咽困难的康复具有治疗潜力。咽部电刺激(PES)是指通过腔内导管直接刺激咽部粘膜,是此类刺激的一个例子。对健康志愿者的早期研究表明,PES在5 Hz和75%的最大耐受强度持续10min可增加咽运动皮层的兴奋性约1h。这些发现表明,外周神经刺激可以在驱动神经系统可塑性方面实现集中效应。一些进一步的研究表明PES在中风后吞咽困难的康复中具有治疗潜力。
尽管人们对神经刺激治疗中风后吞咽困难越来越感兴趣,但现有研究的样本量很小,这限制了对此类干预措施有效性得出明确结论的能力。因此,本文旨在系统地回顾和综合脑卒中后吞咽困难神经刺激随机对照试验(RCT)的证据。在这篇综述中,将重点放在rTMS、tDCS和PES上,因为这些治疗已经证明了从以前的研究中调节神经可塑性的能力。进行亚组分析,以根据随访时间、中风的慢性和刺激模式分析治疗效果,为神经刺激的未来最佳实践提供见解。文章发表在《Neuromodulation: Technology at the Neural Interface》。
本系统评价和荟萃分析遵循系统评价和荟萃分析首选报告项目(PRISMA)指南。两名评审员独立进行了研究搜索、数据提取和偏倚风险评估。数据综合由一名评审员进行,并由第二名评审员验证。从1985年1月到2020年6月,搜索了以下电子数据库:MEDLINE(通过PubMed)、EMBASE(通过Ovid)和Cochrane图书馆。对已鉴定论文的引文进行跟踪,并手动搜索系统评价以查找相关参考文献。用于搜索的术语包括:吞咽困难、吞咽障碍、吞咽障碍、吞咽、吞咽、卒中后、卒中、脑血管意外、梗死、神经刺激、皮质刺激、脑刺激、经颅磁刺激(TMS)、经颅直流电刺激(tDCS),和咽部电刺激(PES)。

研究流程
纳入了所有随机对照试验研究,这些研究比较了神经刺激(rTMS、tDCS和PES)与假刺激或其他干预治疗卒中后吞咽困难(主要是标准护理)的效果。排除病例研究、开放标签研究、动物研究、观察研究、准实验研究、健康志愿者研究和不包括原始数据的研究。非英语研究被排除在外。与吞咽相关的研究结果,包括吞咽生理测量、临床吞咽功能评分、功能性吞咽困难症状量表或与吞咽或咽功能相关的健康结果,以进行比较。
共有638项研究来自三个电子数据库,两项来自其他来源,其中431项研究被认为具有潜在相关性。通过筛选标题和摘要,删除了207项重复研究,排除了391项研究。40项研究进行了资格的全文评估,我们排除了14项研究,原因包括:没有应用目标干预,没有随机对照试验,没有相关性和非相关研究人群的目标结果。26项研究符合纳入标准,并纳入系统分析和荟萃分析。纳入的研究均在2009年至2020年间发表。纳入本荟萃分析的患者总数为852例。在纳入的研究中,13项研究了335名患者的rTMS治疗效果,7项研究了201名患者的tDCS效果,8项研究了316名患者的PES效果。两项研究调查了两种rTMS和PES的效果。患者的平均年龄(SD)为66.0(12.8)岁。从中风发作到干预的时间在不同的研究中有所不同,从30分钟到30分钟不等。
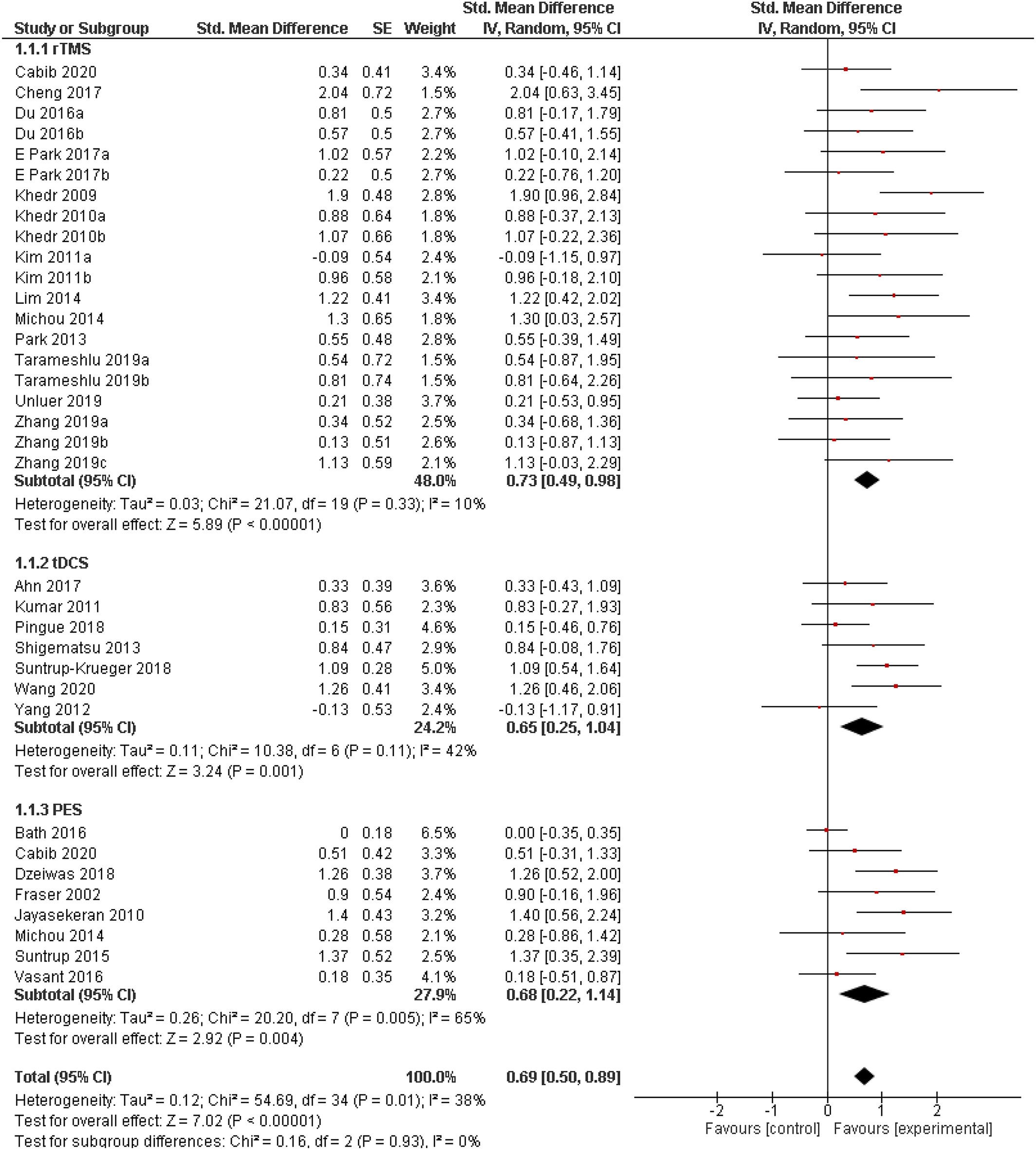
与对照处理相比,显示所有三种治疗方式的总体效果
不同研究中使用的结果测量方法不同。穿透吸入量表(PAS)和吞咽困难结果和严重程度量表(DOSS)是反映吞咽困难严重程度最常用的量表。其他结果测量包括Mann吞咽能力评估(MASA)评分、标准化吞咽评估(SSA)、吞咽困难严重程度分级量表(DSRS)、功能性吞咽困难量表(FDS)、功能性口腔摄入量表(FOIS)、视频荧光透视吞咽困难量表(VDS),吞咽困难分级和吞咽事件发生的时间。两项研究使用准备拔管的患者比例作为结果衡量标准。未拔管的患者被认为有严重吞咽困难,因此治疗失败。因此,这一结果指标被认为是相关的,因为拔管的准备程度与吞咽困难的严重程度密切相关。所有研究均未报告重大不良反应。这些治疗优于传统的吞咽困难治疗或假刺激。所有干预均显示中度效应大小,rTMS显示总体效应大小最大,其次是PES和TDC。在所分析的研究中,未报告重大不良反应。我们的结果表明,在852个样本中,这些神经刺激治疗对卒中后吞咽困难患者是有益的。
结果表明,神经刺激可使脑卒中后吞咽困难患者受益,rTMS和tDCS对单侧刺激最有利的半球不同。这些发现为未来的研究和临床实践奠定了基础。
Cheng, I., Sasegbon, A. and Hamdy, S. (2021), Effects of Neurostimulation on Poststroke Dysphagia: A Synthesis of Current Evidence From Randomized Controlled Trials. Neuromodulation: Technology at the Neural Interface, 24: 1388-1401. https://doi.org/10.1111/ner.13327

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#MET#
73
#卒中后#
75
#Meta#
74
#吞咽困难#
141
#神经刺激#
133