Cell:大脑中存在CD4+T细胞,且影响大脑免疫“哨兵”的发育成熟
2020-07-28 生物探索 生物探索
我们的大脑就像是一个高度设防的总部一样,受到特殊的保护血脑屏障可以防止其他生物大分子进入。同时,有一小部分白细胞可以与血脑屏障相互作用,从而进入大脑血管周隙。也就是说,大脑可能有自己的免疫系统 “哨兵
我们的大脑就像是一个高度设防的总部一样,受到特殊的保护——血脑屏障可以防止其他生物大分子进入。同时,有一小部分白细胞可以与血脑屏障相互作用,从而进入大脑血管周隙。也就是说,大脑可能有自己的免疫系统 “哨兵”。
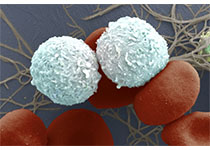
小胶质细胞(microglia)就是大脑中一种常驻免疫细胞,为组织提供固有免疫反应、炎症反应和组织修复。除了小胶质细胞,健康的大脑还应含有血管周围巨噬细胞和树突细胞,以及可检测到的T细胞、B细胞和自然杀伤(NK)细胞。
CD4+T细胞在神经领域是众所周知的自身免疫性疾病的有效介质,如多发性硬化症和嗜睡症等。除此之外,它还在神经退行性疾病中扮演重要角色,如阿尔茨海默症、帕金森、中风等。尽管科学家越来越重视CD4+T细胞在神经炎症和神经退行性疾病过程中的作用,但是CD4+T细胞在健康大脑中是否存在以及潜在功能如何一直存在争议。
为此,由英国巴布拉汉姆研究所(Babraham Institute)和比利时鲁汶(VIB-KU)鲁汶大学(University of Leuven)Adrian Liston教授领导的跨学科科学家团队开始了寻找答案之旅。7月22日,在《Cell》杂志上发表的一项研究中,Adrian Liston等发现,健康的大脑中存在CD4+T细胞,这些细胞影响小胶质细胞的发育成熟。
https://doi.org/10.1016/j.cell.2020.06.026
“对白细胞的误解来自于它们的名字(white blood cells),”Babraham研究所的Oliver Burton博士解释道,“这些‘免疫细胞’不仅存在于血液中。它们不断在我们的身体里循环,并进入我们所有的器官,事实证明也包括大脑。”
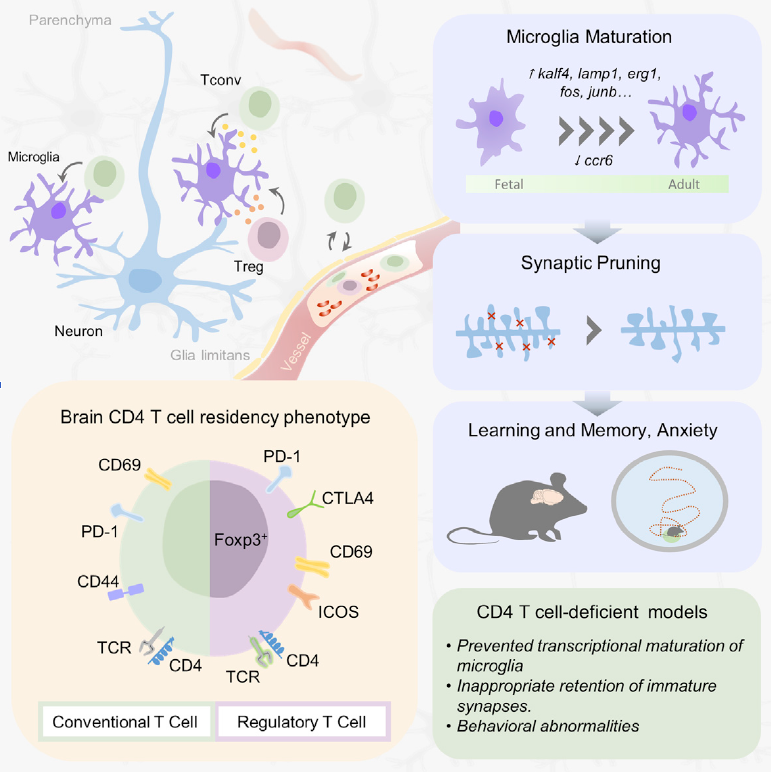
具体来说,研究人员通过显微镜技术和单细胞测序技术等方法,发现在健康的小鼠和人类大脑中CD4+T细胞的存在。CD4+T细胞在脑区中分布相对均匀,且接近小胶质细胞。同时,该研究还量化了小鼠和人类脑组织中的T细胞数量。其中,健康成年小鼠大脑中大约存在2000个CD4+T细胞,其中150个为调节性T细胞。研究人员通过流式细胞术评估了在颞叶手术中切除的健康人脑组织,发现CD4+T细胞的水平与小鼠相似。
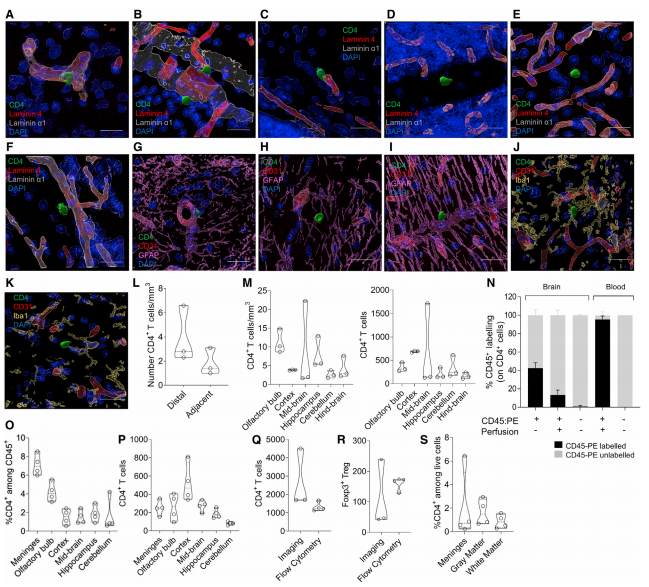
CD4+ T细胞存在于健康的小鼠和人脑中
为了研究脑中CD4+T细胞的具体功能,研究人员转向了MHC II基因敲除(KO)小鼠。这些小鼠在外周和大脑中均表现出CD4+T细胞不足。作为神经系统和免疫系统之间的接口,他们研究了CD4+T细胞缺乏症对小胶质细胞组成的影响。
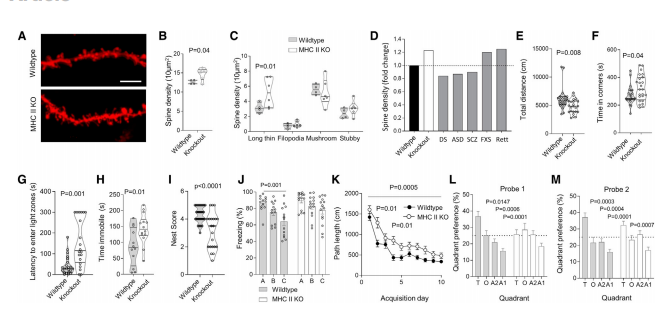
结果显示,当小鼠的大脑中缺乏CD4+T细胞时,那么原本应该在大脑中充当免疫细胞“哨兵”的小胶质细胞就不会完全发育。即CD4+T在脑中小胶质细胞的发育成熟中起作用。观察发现,缺乏CD4+T细胞的小鼠小胶质细胞的形态、数量等似乎没有明显变化,但是成熟小胶质细胞的关键功能——突触剪切受到了干扰,皮层椎体神经元突触密度增加。这些结果表明,CD4+T细胞主要影响成熟小胶质细胞对突触的功能。
此外,这项研究还发现了肠道微生物组之间的联系。研究人员表示,“肠道中的细菌和不同的神经系统疾病之间存在着多种联系,但对于它们之间的联系没有任何令人信服的解释。我们发现肠道细菌会修饰白细胞,然后将这些信息带入大脑。这可能是肠道微生物组影响大脑的途径。”
总结来说,这些发现开启了一系列关于大脑和免疫系统如何相互作用的新问题。这些结果有助于人们越来越多地认识到免疫细胞在大脑中的作用,并对其在一系列神经系统疾病中的作用提供了新的认识。
原始出处:
Emanuela Pasciuto, Oliver T. Burton, Carlos P. Roca, et.al. Microglia Require CD4 T Cells to Complete the Fetal-to-Adult Transition. Cell July 22, 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cell#
73
#CEL#
111
#CD4#
72
#CD4+#
0
#发育#
73
#CD4+T细胞#
114