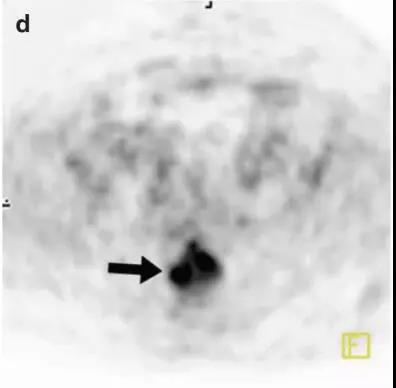
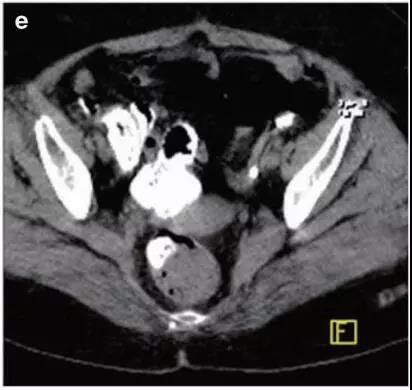
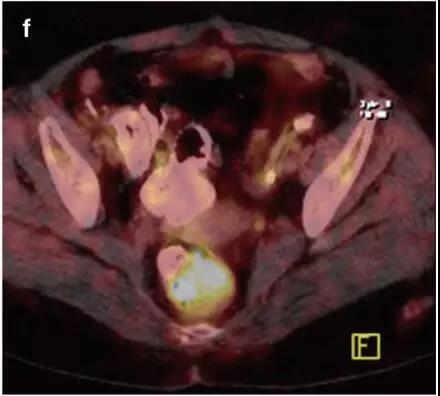
肺癌患者半年后PET/CT复查,发现……
2019-04-27 不详 医学界肿瘤频道
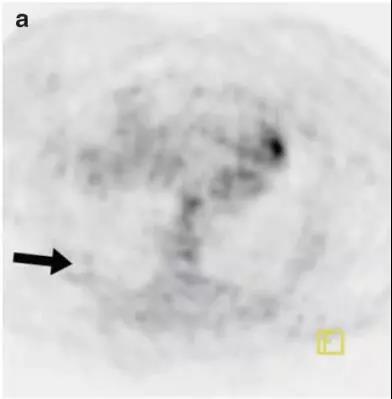
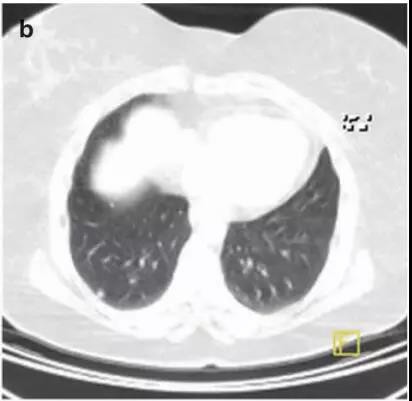
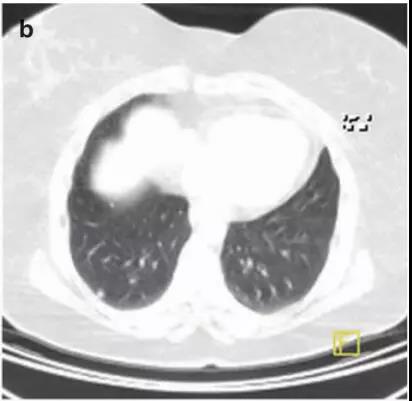
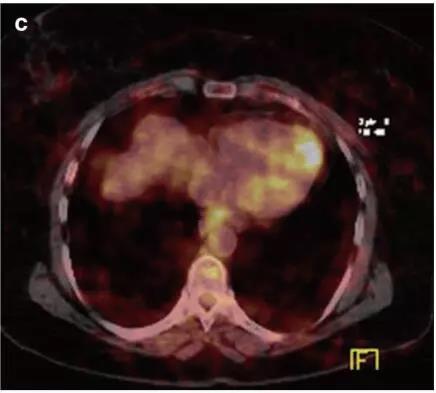
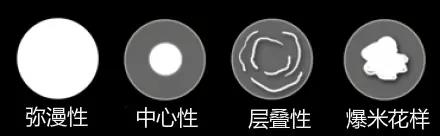
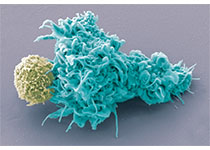
患者,女,54岁,NSCLC治疗后,为再分期行18F-FDG PET/CT检查。由于第一次检查时出现可疑肺结节,因此6个月之后再次行18F-FDG PET/CT检查。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
72
#肺癌患者#
60
#PET/CT#
69
#PET#
59