NCCN肝癌治疗临床指南前沿方案调整解析!新治疗方案生存率如何?
2022-08-02 厚朴方舟 网络
对治疗有缓解的不可切除患者可考虑手术切除,具体的切除标准建议咨询医学肿瘤学家和多学科团队,以确定手术治疗和全身治疗的时机。
肝癌是我国常见的恶性肿瘤,根据国际癌症研究机构(IARC)的统计,2020年我国肝癌新发病例占全球的一半左右。目前,肝癌的治疗方法包括手术、放射治疗、化疗、免疫治疗、靶向治疗等,今年更新的第1版肝癌NCCN指南中,针对肝癌的治疗方案进行了调整。那么,哪些肝癌治疗方案有所改变呢?
▲图源:NCCN指南
手术治疗原则调整
2022年第1版肝癌NCCN指南指出,对治疗有缓解的不可切除患者可考虑手术切除,具体的切除标准建议咨询医学肿瘤学家和多学科团队,以确定手术治疗和全身治疗的时机。
此前,已有多项研究证实,对于一些暂时无法手术的肝癌,也可以经过化疗、靶向治疗、免疫治疗等疗法进行转化治疗后获得手术机会,提高预后。
如,在2018年开展的一项研究中,研究人员就应用索拉非尼治疗FGFR4阳性不可切除肝细胞癌患者,在治疗后成功实施肝肿瘤切除术,术后随访4.5年均无肿瘤复发[2]。
✦
✦
晚期肝癌一线治疗调整
2022年第1版肝癌NCCN指南推荐度伐利尤单抗(2A类证据)、帕博利珠单抗(2B类证据)用于晚期肝癌一线治疗。
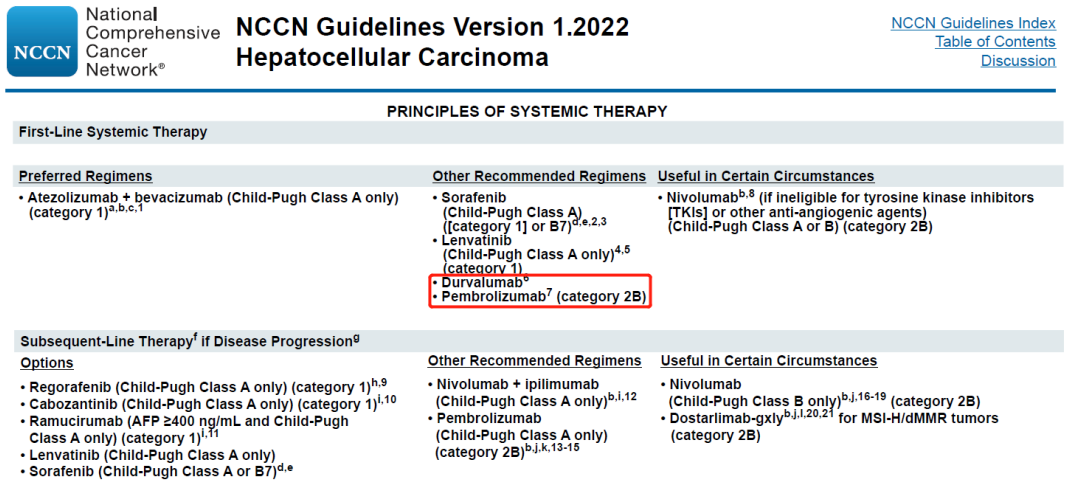
HIMALAYA III期研究评估了采用度伐利尤单抗+Tremelimumab(D+T)、度伐利尤单抗单药或索拉非尼一线治疗肝癌患者的效果。研究结果显示,与索拉非尼(S)相比,D+T组合疗法和度伐利尤单抗单药(D)均显著改善了肝癌患者的生存期(D+T vs D vs S:16.4 vs 16.6 vs 13.8个月)[3]。
KEYNOTE-224此前公布的数据已经证实帕博利珠单抗单药治疗在既往接受索拉非尼治疗的晚期肝癌患者中效果显著。2021年研究人员公布了采用帕博利珠单抗一线治疗晚期肝癌的效果。结果显示,客观缓解率为16%,疾病控制率为17%;1年无进展生存率为24%,中位无进展生存期为4个月;1年总生存率为58%,中位总生存期为17个月[4]。
✦
✦
晚期肝癌二线治疗调整
2022年第1版肝癌NCCN指南推荐雷莫芦单抗(雷莫西尤单抗,Cyramza)仅用于AFP≥400ng/ml以及Child A级的肝细胞癌患者(1类推荐)。
2019年,美国FDA批准雷莫芦单抗(Cyramza)用于治疗甲胎蛋白(AFP)≥400ng/mL且已接受过索拉非尼治疗的肝细胞癌(HCC)患者。
REACH-2 (NCT02435433)研究结果显示,接受雷莫芦单抗治疗的肝癌患者生存期显著延长(中位OS:8.5个月 vs 7.3个月)[5]。
✦
✦
目前,针对肝癌治疗的方案越来越多,效果也越来越显著,即使是无法手术的肝癌患者也可以在合理的治疗后获得长期生存。但是,每一种疗法都有其适应症要求,对于肝癌的治疗,需要根据患者的病情,量身定制合适的治疗方案。
- END -

版权声明:本文为厚朴方舟原创内容,版权归厚朴方舟所有,欢迎转发朋友圈,任何公众号或其他媒体转载必须注明来源于【厚朴方舟】(ID:hope-noah)或者后台联系小编开白名单。
免责声明:本公众号内容仅作交流参考,不作为诊断及医疗依据,专业医学问题请咨询专业人士或专业医疗机构。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#临床指南#
82
#解析#
92
#治疗方案#
112
好文章,值得一读。
74
#肝癌治疗#
166
#生存率#
143
#NCCN#
111