ASCO-GU 2018:寡转移性前列腺癌的临床处理
2018-02-13 作者 | 纪长威 郭宏骞(南京大学医学院附属鼓楼医院泌尿外科) 编辑 | 豆豆(中国医学论坛报) 中国医学论坛报今日肿瘤
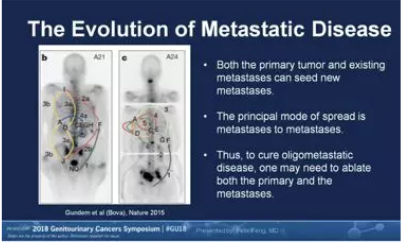
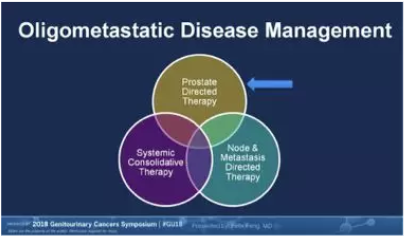
2018年ASCO GU研讨会于当地时间2月8日在旧金山拉开帷幕,吸引了超过4300名来自世界各地的泌尿生殖肿瘤专家和基础研究学者参与。论坛首日的内容是关于前列腺癌的临床和基础研究进展,寡转移性前列腺癌(Oligometastatic Prostate Cancer)的诊疗是本次论坛的讨论热点之一。



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#临床处理#
63
#ASC#
57
#转移性#
72
#转移性前列腺癌#
72
寡转移照样手术处理
111
学习一下很不错
93