JCO:非小细胞肺癌患者抗PD-1/PD-L1阻断治疗反应的分子决定因素
2018-01-18 MedSci MedSci原创
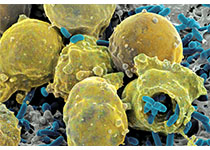
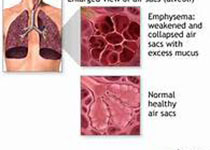
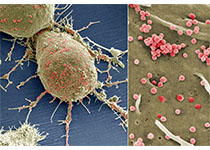
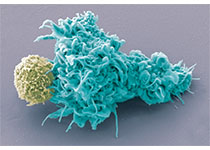
使用免疫检查点抑制(ICI)治疗晚期非小细胞肺癌有持续的治疗反应,可以改善患者预后。目前尚需最大化ICI作用的临床工具以及进一步理解治疗反应的分子决定因素。二代测序(NGS)技术正变得越来越普遍,但是其在发掘ICI治疗反应预测分子领域的作用尚未知。JCO近期发表了一篇文章,研究了这一问题。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肺癌患者#
56
#JCO#
54
#阻断#
57
#非小细胞#
72
#决定因素#
62
#PD-L1#
50
#非小细胞肺癌患者#
57
学习了.涨知识
102
学习谢谢分享
93