CSCO 2021:秦叔逵教授报告阿可拉定一线治疗基线较重预后较差晚期肝细胞癌结果
2021-09-25 MedSci原创 MedSci原创
阿可拉定主成分是淫羊藿苷元(anhydroicaritin),为类黄酮类化合物,别名为脱水淫羊藿素,天然存在于小檗科植物淫羊藿中,但含量很低。目前,淫羊藿苷元主要以淫羊藿苷为原料,采用酶解法、酸解法、
阿可拉定主成分是淫羊藿苷元(anhydroicaritin),为类黄酮类化合物,别名为脱水淫羊藿素,天然存在于小檗科植物淫羊藿中,但含量很低。目前,淫羊藿苷元主要以淫羊藿苷为原料,采用酶解法、酸解法、酶解酸解相结合法及化学合成法制备。
肝细胞癌(hepatocellular carcinoma,HCC)占肝原发性肿瘤九成,具有高发病率、高致死率的特点,是全球性人类重大疾病。研究显示,阿可拉定在人肝细胞癌细胞系中具有抑制肿瘤生长、抑制肿瘤细胞活力、诱导细胞凋亡等作用,是潜在的小分子靶向药物。
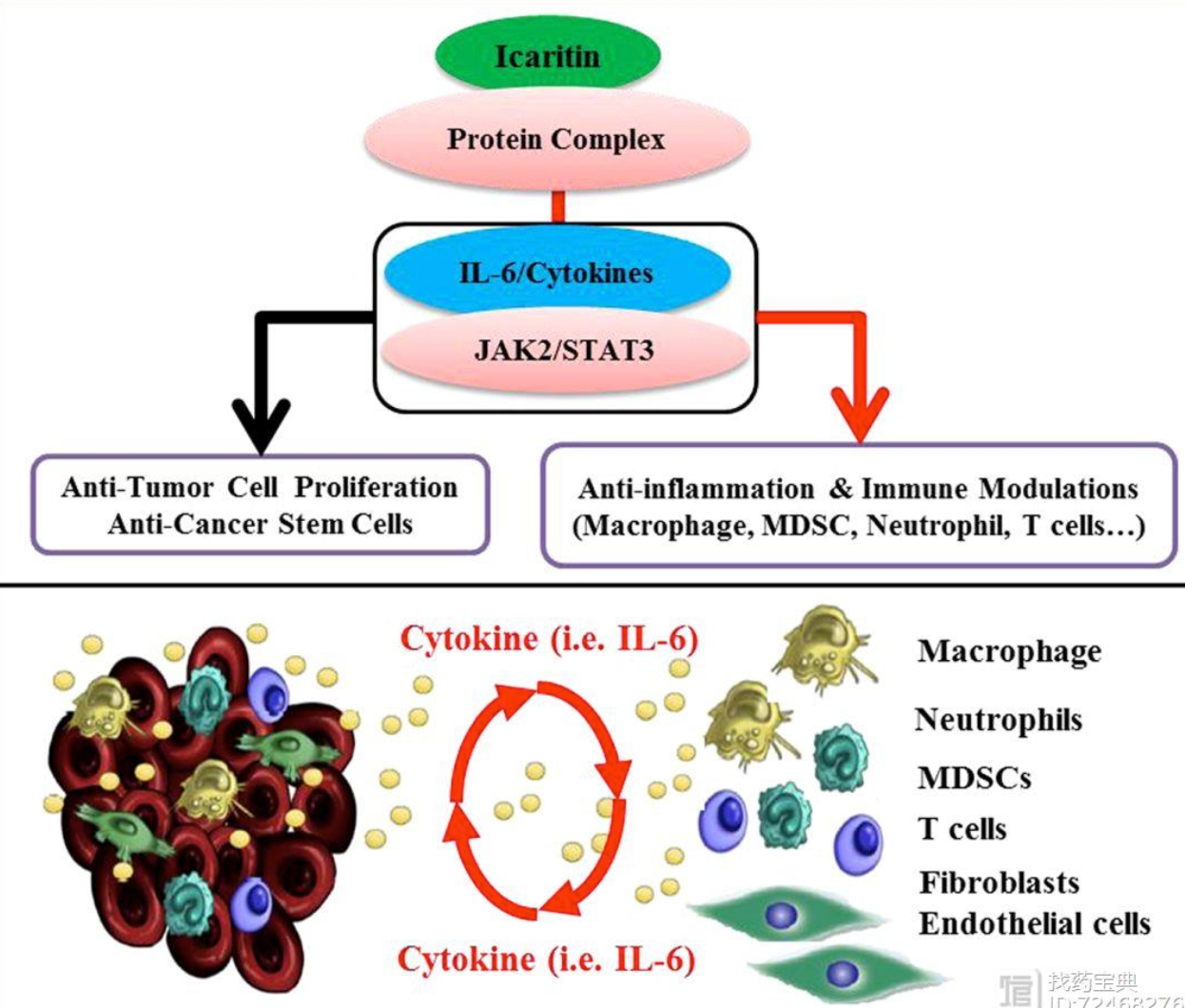
在抗肝癌作用机制上,阿可拉定主要是通过IL-6/STAT3、IGF1/STAT3、MAPK/ERK等信号通路发挥作用,抑制肿瘤细胞增殖,降低细胞活力,诱导肿瘤细胞大量凋亡;此外,阿可拉定还具有免疫调节功能,能诱导免疫抑制细胞分化,降低免疫抑制水平。研究证明,超六成肝癌患者显示STAT3高度激活,STAT3激活同时预示着肝细胞癌较高的恶性程度。利用肝细胞特异性敲除STAT3小鼠研究二甲基亚硝胺诱导肝细胞癌模型的研究结果显示:肝细胞特异性敲除STAT3小鼠的肝细胞癌发生率比对照组低6倍,并且肿瘤体积较小,说明STAT3与肝细胞癌细胞增殖存活密切相关。阿可拉定可作用于STAT3相关通路,也正是其抗肝癌的关键所在。
此外,阿可拉定还被用于黑色素瘤、T淋巴细胞瘤、肾细胞癌、乳腺癌、前列腺癌、子宫内膜癌等多种肿瘤疾病的治疗。其作用机理如图二所示,具体来说:抗黑色素瘤主要通路为IL-6/JAK/STAT3;抗T淋巴细胞瘤主要通路为JAK/STAT3和PI3K/AKT通路;抗肾细胞癌主要通路为JAK/STAT3;抗乳腺癌主要通路为MAPK/ERK;抗前列腺癌主要靶点为Androgen Receptor(AR)Signal;抗子宫内膜癌主要通路为MAPK/ERK。
前不久,国际癌症学术期刊Cancer Science(《癌症科学》)在线发表盛诺基天然小分子阿可拉定免疫调节治疗晚期肝细胞癌II期临床试验结果: “Icaritin Induced Immunomodulatory Efficacy in Advanced HBV-Related Hepatocellular Carcinoma: Immunodynamic Biomarkers and Overall Survival” (DOI:10.1111/cas.14641)。该研究由我国著名肿瘤专家孙燕院士和秦叔逵教授牵头,由全国多家医院临床研究中心合作完成。阿可拉定是从传统中药淫羊藿分离的淫羊藿提取物经酶解产生的小分子药物,具有多靶点抗炎症及抗肿瘤免疫调节生物学活性,在中国晚期肝细胞癌临床I/II期试验中得到了安全性及疗效的初步验证。在中国晚期肝细胞癌患者II期临床试验中(入组患者HBV感染占91.2%)显示了相对于传统靶向药和免疫检测点抑制剂显著的安全性优势,未观察到严重的3/4级不良事件, 而且具有显著的抗炎症及抗肿瘤免疫调节临床疗效特征。晚期肝细胞癌患者服用阿可拉定后免疫生物标志物动态变化与生存期延长显著相关,获益患者中位生存区间可达329-565天。晚期患者复合标志物包括高表达AFP及免疫细胞相关因子与临床获益生存呈显著相关趋势,为阿可拉定治疗预后较差晚期肝细胞癌患者带来新希望。
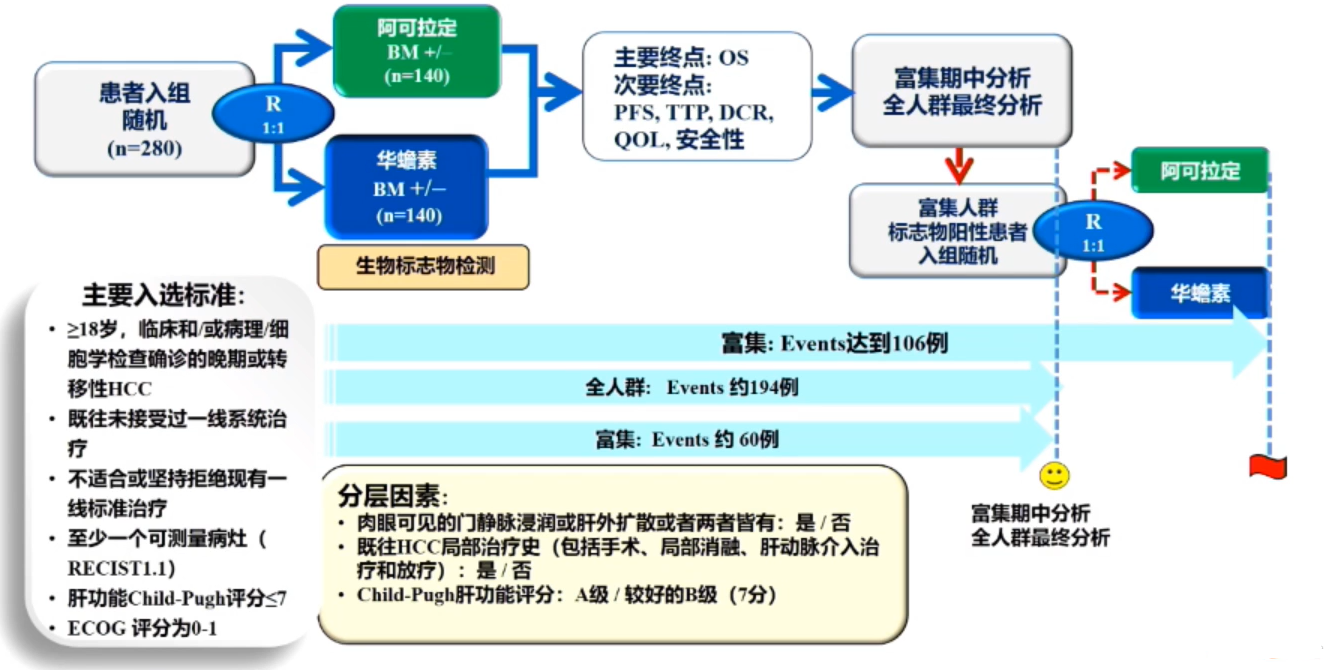
据悉,此次阿可拉定针对肝癌的三期临床研究是经我国药品监督管理局(NMPA)批准,由中国工程院院士孙燕和南京中医药大学附属八一医院秦叔逵共同牵头,组织了全国28家研究中心联合开展。该临床实验采用了复合生物标志物适应性富集设计,目前已经入组晚期肝细胞癌共280余例。现有结果显示,阿可拉定主要疗效终点总生存(OS)期达到了预设的优效界值,与对照组相比具有显著的生存优势,且安全性和耐受性良好。
在刚刚开幕的CSCO大会上,在大会主题报告中,秦叔逵教授为我们带来了肝癌领域的最新研究,即“阿可拉定一线治疗基线较重预后较差晚期肝细胞癌的多中心、随机、双模拟Ⅲ期临床研究结果:标志物富集设计、总生存、生活质量及安全性”。该药物对比华蟾素一线治疗晚期肝细胞癌患者的有效性、安全性的前瞻性、随机对照、双盲双模拟、全国多中心的临床III期试验达到了主要终点,显示阿可拉定上市指日可待。
研究纳入280例既往未接受过一线系统治疗的晚期或转移性HCC患者,按1:1随机接受阿可拉定或华蟾素治疗,同时进行生物标志物检测。研究主要终点为OS,次要终点为无进展生存(PFS)、至进展时间(TTP)、疾病控制率(DCR)、生活质量(QOL)和安全性。分层因素包括肉眼可见的门静脉浸润成肝外扩散,既往HCC局部治疗史以及Child-Pugh肝功能评分。富集期中时进行分析,在阳性情况下对全人群最终分析,特别注意富集人群标志物阳性患者的结果(图2)。
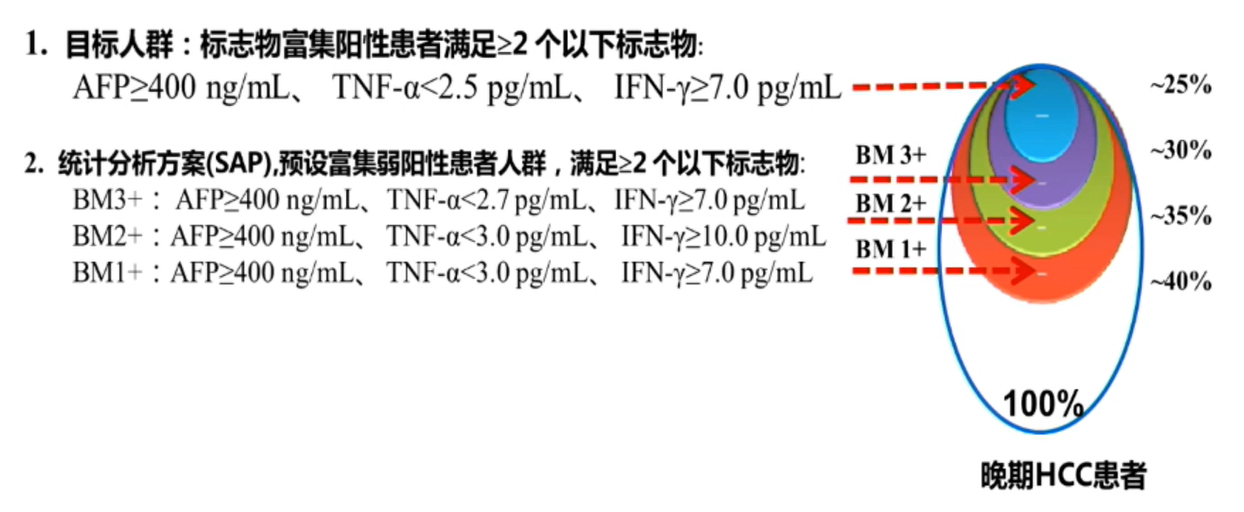
富集人群的基线特征显示,患者的疾病分期更晚,病情更为复杂,例如肉眼可见的门静脉浸润或肝外扩散或两者都有的患者占60%以上,AFP≥400ng/mL的患者占80%以上等,患者预后较差,相当多的患者不能接受化疗、靶向或免疫等现有治疗
富集人群临床疗效显示,阿可拉定组的中位OS显著优于对照组,分别为13.54 vs 6.87个月(HR=0.43,P=0.0092),降低死亡风险57%(图3)。同时,在不同等级阳性晚期HCC人群中均显示,阿可拉定组的中位OS优于对照组(图4),这也验证了富集标志物预测阿可拉定临床疗效的可靠性。研究期间未接受标准HCC系统治疗,但疾病进展(PD)后继续用药的富集人群中,阿可拉定组的中位OS对比对照组显著延长,分别为18.97个月vs 11.43个月(HR=0.14,P=0.0094)。
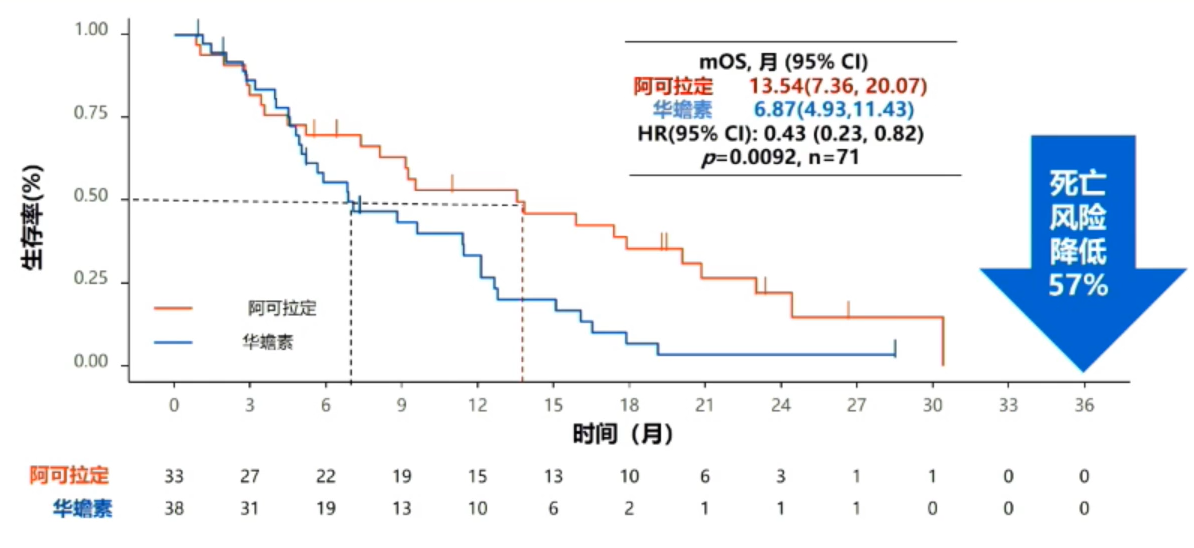
富集人群临床疗效:OS
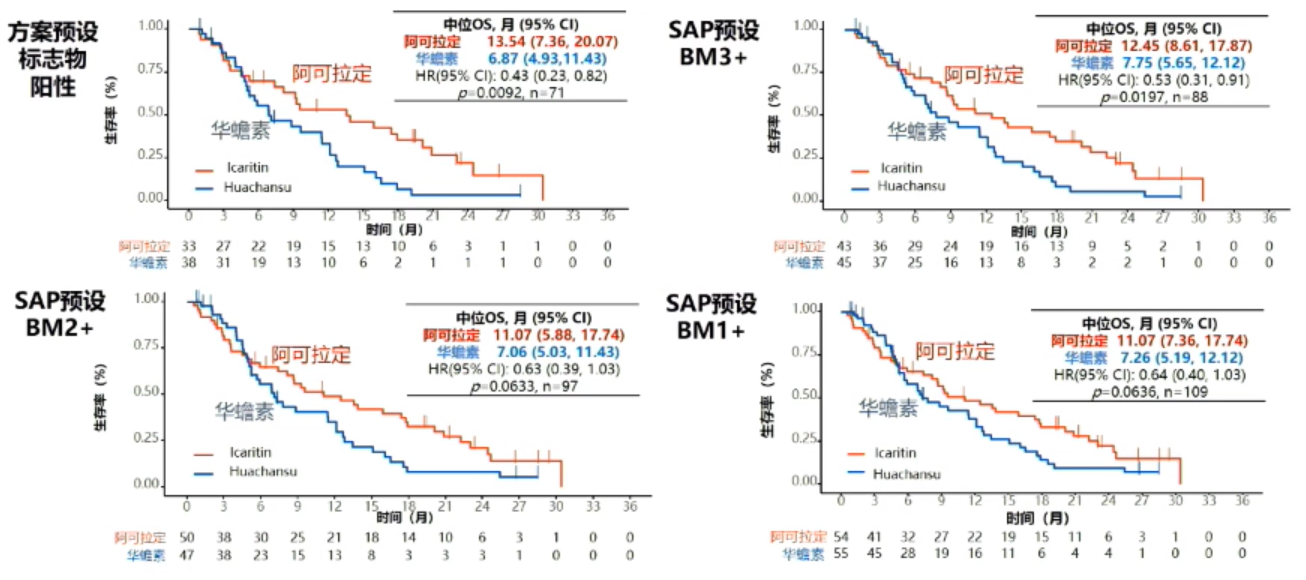
不同富集人群的OS结果
阿可拉定组中研究者评估的中位TTP和中位PFS未见明显差异,但均较对照组有改善的趋势(图5),这可能与研究样本量较小有关,也与阿可拉定起效较慢、时间较为持久有关。
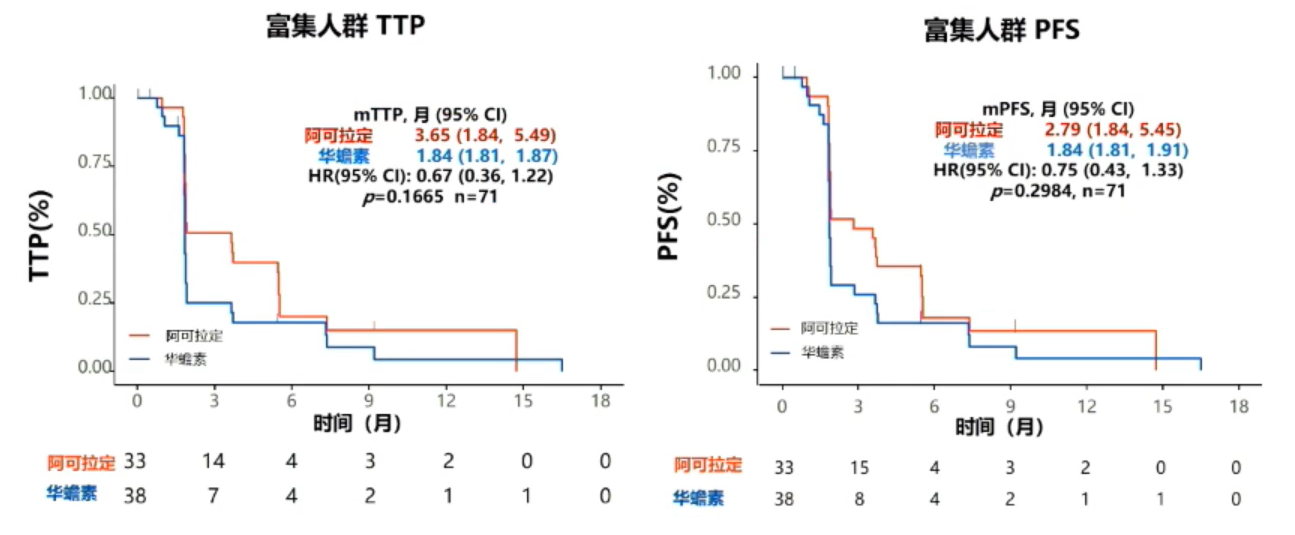
富集人群:TTP和PFS
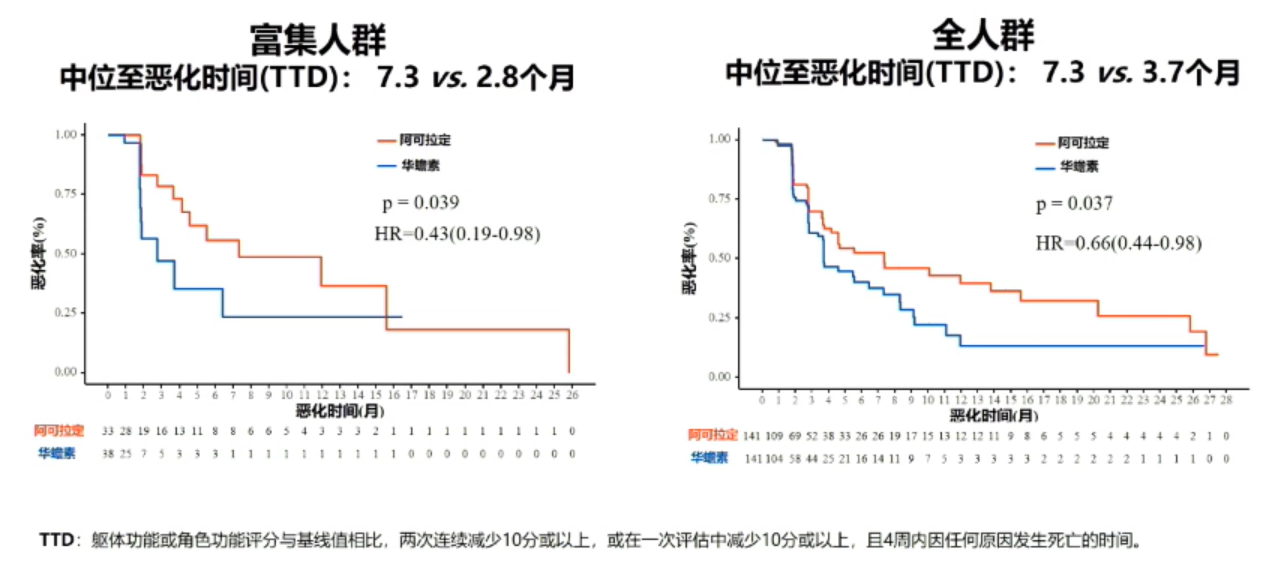
在QOL方面,富集人群中位至恶化时间(TTD)在阿可拉定组与对照组分别为7.3个月vs 2.8个月,在全人群组中,两组的中位TTD分别为7.3个月vs 3.7个月(图6)。因此,与华蟾素组相比,阿可拉定组的患者生活质量得到显著提高。
与药物相关的不良事件显示,全人群及富集人群中,阿可拉定的安全性均优于华蟾素,治疗相关不良事件(TRAE),≥3级TRAE、导致永久性停药以及剂量调整的TRAE、与研究药物相关的严重不良事件(SAE)发生率,阿可拉定组均明显低于对照组。
总之,口服免疫调节药物阿可拉定对比华蟾素一线治疗晚期HCC,显著延长总生存,并显著改善患者生活质量,延长中位至恶化时间。此外,阿可拉定治疗晚期HCC患者具有显著的安全性优势,疾病进展后继续用药仍可延长总生存;其总体不良反应发生率及≥3级不良反应发生率均低于现有的一线治疗药物。外周血复合标志物可以预测阿可拉定临床疗效,为晚期HCC患者提供精准治疗选择。
目前阿可拉定用于既往未接受过全身系统性治疗的不可切除的肝细胞癌,已获CDE优先评审资格。
另外,阿可拉定对比索拉非尼一线治疗PD-L1阳性晚期肝细胞癌患者的随机、开放性临床试验研究也正在进行中。根据前期临床研究中发现的PD-L1与阿可拉定临床疗效的相关性及阿可拉定机制研究结果,将患者基线肝癌组织免疫细胞中PD-L1的表达阳性纳入入组标准。在PD-L1阳性患者中,对比阿可拉定与目前晚期肝细胞癌的标准治疗索拉非尼,其主要疗效和安全性终点与第一项研究基本一致。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#秦叔逵#
84
#细胞癌#
68
#肝细胞#
73
#阿可拉定#
86
#晚期肝细胞癌#
84
了解一下
106
时刻学习
103
期待后续更多的消息
108