双支架套叠植入术治疗以三叉神经痛起病的椎-基底动脉延长扩张症1例报告并文献复习
2018-12-13 穆振欣 郑栋 杨钟熙 中风与神经疾病杂志
椎-基底动脉延长扩张症(vertebrobasilar dolichoectasia,VBD)是一种以椎-基底动脉显著扩张、延长、扭曲或成角为特征的少见的脑血管异常性疾病。普通人群发生率为0.06%~5.8%。该病病因尚未完全明确,临床表现复杂多样,诊断主要依据影像学特征。VBD的治疗尚无疗效肯定的方案,临床主要侧重于内科对症治疗和外科手术干预处理扩张血管,现将我院双支架套叠植入术治疗三叉神经痛起
椎-基底动脉延长扩张症(vertebrobasilar dolichoectasia,VBD)是一种以椎-基底动脉显著扩张、延长、扭曲或成角为特征的少见的脑血管异常性疾病。普通人群发生率为0.06%~5.8%。该病病因尚未完全明确,临床表现复杂多样,诊断主要依据影像学特征。VBD的治疗尚无疗效肯定的方案,临床主要侧重于内科对症治疗和外科手术干预处理扩张血管,现将我院双支架套叠植入术治疗三叉神经痛起病的VBD1例报告如下。
1.临床资料
患者,男性,50岁,因“发作性右侧面部刺痛7y余”入院。患者近7y在咀嚼、刷牙等面部活动时经常出现右侧面部刺痛,以三叉神经眼支及上颌支支配范围为主,每日发作约2~3次,每次持续约1~2min,给予卡马西平口服,从200mg/d逐步加量至600mg/d,患者症状缓解后又加重。
辅助检查:入院前头CTA、MRA见右侧椎动脉颅内段明显扩张,基底动脉呈不规则瘤样扩张,走形迂曲(见图1、图2)。

图1 右侧椎动脉颅内段明显扩张,基底动脉呈不规则瘤样扩张,走形迂曲
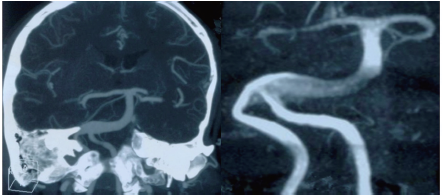
图2 右侧椎-基底动脉明显增粗,显影浅淡,椎-基底动脉延长扩张症
入院后查头部高分辨率核磁、DSA示双侧椎动脉及基底动脉走形迂曲,管壁略厚。基底动脉起始部管腔明显增粗、其内可见血流信号伪影,桥脑右部明显受压,增粗部位未见明显双腔影(见图3、图4)。
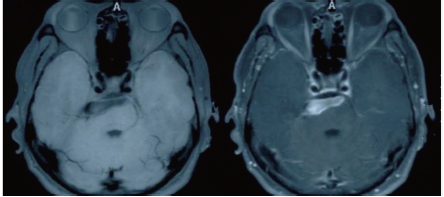
图3 基底动脉起始部管腔明显增粗、其内可见血流信号伪影,桥脑右部明显
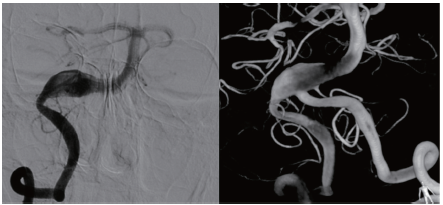
图4 右侧椎动脉颅内段及基底动脉明显增粗,增粗部位未见明显双腔影
入院后诊断为椎-基底动脉延长扩张症,右侧三叉神经痛。治疗及预后:全麻下将第一枚LVIS Intraluminal Support 5.5mm/25mm支架头端锚定于基底动脉-右侧椎动脉移行处,尾端释放于右侧椎动脉扩张处,第二枚LVIS Intraluminal Support 5.5mm/25mm支架头端锚定于第一枚支架后1/3处,两枚支架将椎-基底动脉扩张处完整覆盖。
术后右侧面部刺痛仍有刺痛表现,但程度及频率较术前减少。术后6m三叉神经痛症状消失,复查DSA示:扩张的椎-基底动脉以支架为骨架重塑,扩张血管壁回缩,血管基本回到正常结构形态(见图5),随访1y未见复发。
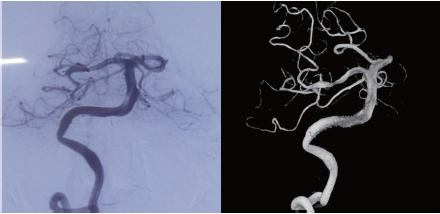
图5 扩张的椎-基底动脉以支架为骨架重塑,血管壁回缩,基本回到正常结构形态
2.讨论
椎-基底动脉延长扩张症(vertebrobasilar dolichoectasia,VBD)是一种临床上相对少见的疾病,曾先后被命名为“巨大延长的基底动脉瘤畸形”、“血管曲张样动脉瘤”和“梭形动脉瘤”等。20世纪80年代,Smoker等对126例患者行头部CT检查分析后,将其命名为VBD。关于VBD的发病机制目前没有明确统一的理论,曾经认为高血压、糖尿病等引起的动脉粥样硬化的危险因素是导致VBD的主要病因,但随着动脉粥样硬化与VBD的发病率的不同等新证据的出现,该理念被逐渐否定。
现在人们认为VBD的发病机制主要为遗传因素导致肌纤维发育异常,从而导致动脉内弹力层缺如、纤细和(或)平滑肌层萎缩有关。该机制看似与动脉粥样硬化病因相似,但两者早期病理改变不同,动脉粥样硬化以脂质浸润、内膜增生为主,而VBD以弹力层破碎变薄为主要病理改变。
VBD患者可无任何症状,仅在体检时发现,也可以表现为复杂的症状,主要可以概括为以下四类。
(1)缺血性脑卒中:是VBD最常见的死因,引起该症状的可能原因有:①扩张的椎-基底动脉内血流方向、速度改变引起的供血区脑灌注不足;②扩张血管对内皮细胞的损伤;③扩张血管内形成的血栓斑块脱落;④周围小血管牵拉引起的周围脑组织缺血。
(2)出血性脑卒中:该症状相对少见,考虑为扩张的动脉血管内弹力层缺如、纤细和(或)平滑肌层萎缩破裂等病理改变引起动脉破裂出血。
(3)脑积水:延长扩张动脉内的血流博动对第三脑室底部或者Monro孔产生一种“水锤效应”,导致脑积液的流出受阻引起的梗阻性脑积水为该症状发生的主要原因,同时VBD的直接机械压迫同样可以引起该症状。
(4)脑干及脑神经受压所产生的症状:该症状为扩张血管产生的占位效应对脑干及脑神经压迫所产生,其中面神经和三叉神经是最常受累及的脑神经。该患者三叉神经痛起病,三叉神经痛病因多种多样,其中三叉神经脑池段的神经血管压迫或接触引起刺激症状是原发性三叉神经痛的主要原因。
扩张的椎-基底动脉压迫或接触是引起该患者三叉神经痛症状的原因。VBD的诊断主要依靠影像学检查,其中Smoker等提出的CT、CTA诊断标准:当基底动脉分叉高度达到或超过鞍上池且基底动脉直径≥4.5mm,即可诊断为VBD。由Ubogu等提出的MRA诊断标准:基底动脉长度>29.5mm,或基底动脉上段超过鞍上池或床突平面6mm即为延长,椎动脉颅内段度>23.5mm即为延长。该诊断标准是目前临床上常用的诊断依据。
高分辨率核磁作为新兴的检查手段对于VBD是否合并夹层的鉴别诊断具有一定的意义。DSA作为诊断VBD的金标准,不但能最直观的展现出椎-基底动脉扩张的形态,同时可以明确椎-基底动脉是否合并有夹层、动脉瘤、动脉狭窄等病变,这对于VBD治疗方案的选择及预后判断具有重大的意义。该患者以顽固性三叉神经痛起病,入院后CTA及MRA检查结果均符合诊断标准,高分辨率核磁明确椎-基底动脉扩张对桥脑右部的压迫,DSA检查明确诊断。
综上患者临床VBD诊断明确。VBD目前没有确切有效的治疗方案。临床上常见的治疗方式有:
(1)抗凝、抗血小板等内科治疗预防后循环卒中。Flemming等认为使用抗凝或抗血小板药物可以减少缺血性脑卒中复发率,可以使患者受益,这也是目前对于VBD最常见的治疗方案。
(2)采用单侧的脑室-腹腔分流术、双侧脑室-腹腔分流术内镜下第三脑室底造瘘术等方案治疗VBD引起的脑积水。
(3)微血管减压术(microvascular decompression,MVD),解除脑干及脑神经受压的症状。但是在扩张血管和脑干之间植入人工补片不但缓解不了脑干受压,相反还会加重压迫以及解剖、手术风险等因素,该术式受到一定限制。
(4)介入治疗,该术式是近年新兴的治疗方式。通过支架辅助治疗动脉瘤的经验,血管内支架植入可以改变血流动力学,减轻血流对动脉瘤的冲击,这为血管内支架植入治疗VBD提供了理论基础。
有报道成功应用支架套叠置入有效治疗VBD,这为椎动脉延长扩张的血管内治疗可行性提供了依据。但是因为椎-基底动脉解剖特点,套叠支架的植入可能影响其穿支的血供,该治疗方案仍存在风险。
随着介入材料的发展及介入技术的更新,根据血管长度、内径及扭曲程度选择合适的支架,采用多支架套叠植入增加支架覆盖率,改变局部血流,减少血流对病变血管的冲击,为病变血管修复提供条件。根据支架套叠置入治疗VBD的理论及技术支持,使这一治疗方案成为现实。其优点有:(1)在扩张的血管内植入支架可以使扩张动脉内血流动力学发生改变;(2)密网支架及重叠释放多枚支架技术的应用可以减轻血流对于血管壁的冲击作用;(3)植入的支架可以作为新的骨架被新生的组织填塞从而形成新的管腔,同时以支架为骨架新生成的管腔更符合正常血管的形态;(4)扩张的血管因机化等复杂变化逐渐回缩,使扩张的血管逐渐回归到相对正常的血管形态,从而使脑干及脑神经受压得到缓解,同样可以缓解脑积水;(5)支架的植入可以减少缺血及出血性脑卒中事件的发生。该患者主要以脑神经受压而引起的三叉神经痛起病,桥脑右部受压明显。
经系统的内科治疗后症状无缓解反而逐渐加重,完善术前评估后根据病变血管的特点,予以套叠的方式植入2枚LVIS Intralumina lSupport 5.5mm/25mm支架治疗。患者术后6m入院复查,三叉神经痛症状基本消失,DSA复查较术前示:双支架覆盖的扩张椎-基底动脉明显回缩,扩张血管得到明显重塑,扩张的血管基本回到正常形态(见图5)。术后1y电话随访,患者三叉神经痛症状完全消失。该患者VBD得到有效治疗。综上,结合该病例,在临床上当我们遇到脑神经受压为主要症状的VBD患者经过系统的内科治疗,患者症状无缓解甚至逐渐加重的患者,可考虑行VBD的多支架介入治疗。通过对本病例的治疗,作者认为使用多支架套叠置入术治疗VBD的方法可行,长期效果有待于进一步临床观察及增加病例研究。
原始出处:
穆振欣,郑栋,杨钟熙,陈儇,罗祺.双支架套叠植入术治疗以三叉神经痛起病的椎-基底动脉延长扩张症1例报告并文献复习[J].中风与神经疾病杂志,2018,35(01):59-60.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#三叉神经#
72
#扩张#
94
#三叉神经痛#
89
#植入#
63
#神经痛#
67
#基底动脉#
96