PLoS One:原发性甲状旁腺功能亢进症患者甲状旁腺切除术后的急性和长期肾功能
2021-01-18 AlexYang MedSci原创
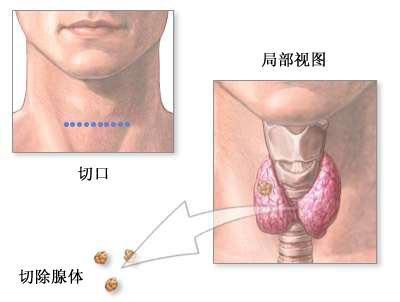
在肾移植患者中,甲状旁腺切除术与肾功能急性下降有关。在原发性甲状旁腺功能亢进症(PHPT)患者中,甲状旁腺切除术对肾功能的急性和慢性影响尚未得到广泛的研究。
在肾移植患者中,甲状旁腺切除术与肾功能急性下降有关。在原发性甲状旁腺功能亢进症(PHPT)患者中,甲状旁腺切除术对肾功能的急性和慢性影响尚未得到广泛的研究。
最近,有研究人员进行了一项回顾性队列研究,包括了494名因PHPT接受甲状旁腺切除术的患者。研究共包括了391名(79.1%)女性患者,422名(85.4%)非非裔美国人,年龄中位数为58岁。术前血清肌酐、PTH和总钙水平中位数(第一和第三分位数)分别为0.81 mg/dL(0.68-1.01)、154.5 pg/mL(106-238.5)和10.9 mg/dL(10.3-11.5)。术前eGFR的中位数(第一和第三四分位数)为86 mL/min/1.73 m2(65-101.3)。术后,eGFR急性下降的中位数为21 mL/min/1.73 m2(P<0.0001)。41.1%的患者发展为1期AKI,5.9%发展为2期AKI,1.8%发展为3期AKI。单变量分析中,急性eGFR下降(%)与年龄和PTH、钙和术前肌酐水平相关。多变量分析显示,急性变化与年龄和术前离子钙、磷和肌酐值有关。12个月的变化与性别、术前肌酐和25OHD有关。60.7%的患者在急性发作后发生eGFR永久性降低。

基于PHPT病因分层的估算肾小球滤过率(eGFR)的均值和标准差变化
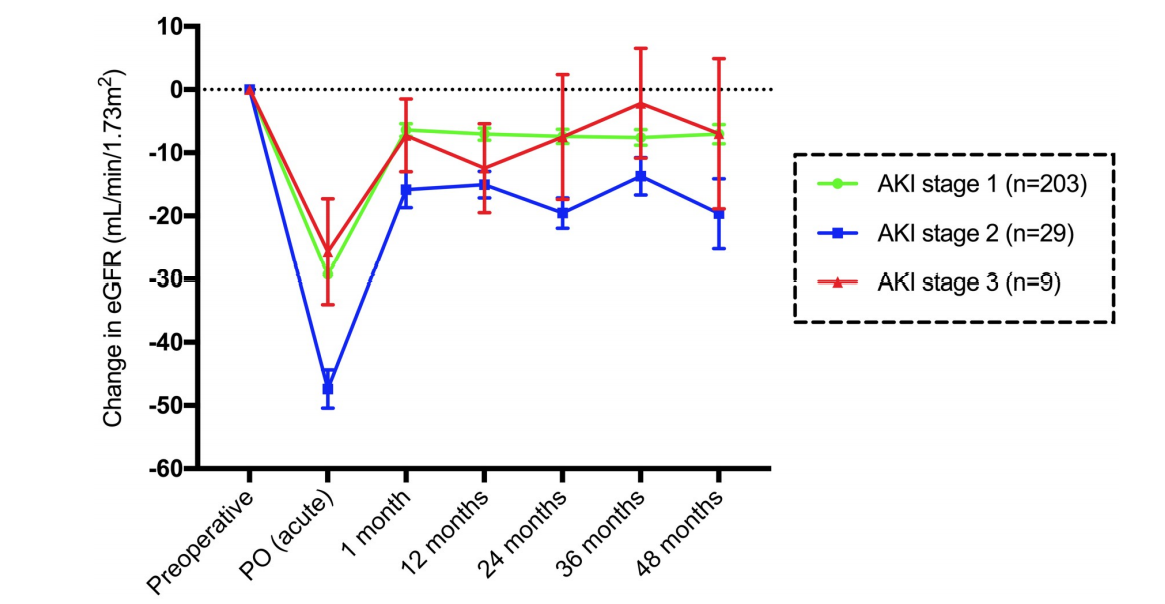
基于急性肾损伤阶段的eGFR均值和标准差变化
最后,研究人员指出,PHPT甲状旁腺切除术后肾功能有明显的急性损害,近一半的患者符合AKI的标准。术后第一个月能够观察到明显的eGFR恢复,但可能会出现部分患者的永久性降低。与接受甲状腺切除术的患者相比,接受PHPT治疗的患者似乎出现了明显的肾功能障碍。
原始出处:
Marcelo Belli , Regina Matsunaga Martin , Marília D'Elboux Guimaríes Brescia et al. Acute and long-term kidney function after parathyroidectomy for primary hyperparathyroidism. PLoS One. Dec 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Plos one#
73
#肾功能#
61
#原发性#
56
#切除术#
63
#甲状旁腺功能亢进#
73
#甲状旁腺#
0
#甲状旁腺切除术#
61
#原发性甲状旁腺功能亢进#
61