Nature:两篇论文挑战癌症干细胞概念:癌干细胞与癌症转移有关吗?
2017-04-02 万纹 生物通
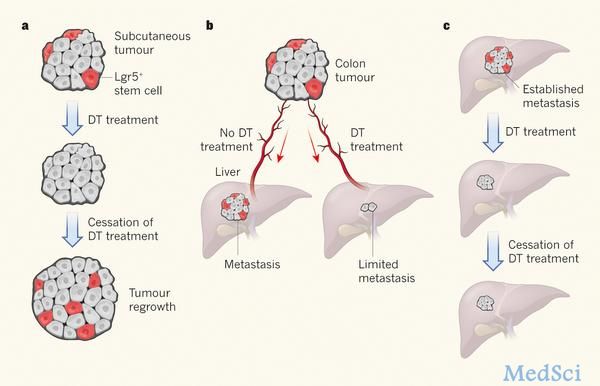
科学家们认为干细胞分裂是肿瘤生长所必需的,癌症干细胞能驱动肿瘤生长与转移,由此提出了将去除癌症干细胞作为癌症治疗的靶标之一。然而这在许多类型的癌症中都还没有找到确凿的实验证据。最新一期(3月29日)Nature杂志中,来自日本和美国的科学家通过靶向去除特殊的干细胞群体,发现了这些干细胞在肿瘤发展中的作用,以及对于癌症转移的影响。Lgr5+干细胞小肠上皮细胞层是哺乳动物机体的自我更新支持者,它的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
98
下次可否把DOI加上,谢谢
106
#癌症干细胞#
128
#癌症转移#
77
#癌干细胞#
76
肿瘤干细胞是化疗耐药的根本原因
126
学习了,多谢分享
134
受教了,谢谢分享,已收藏
92
学习了
96