中药汤剂可延长IV期食管鳞状细胞癌诊断后的寿命
2022-06-16 August MedSci原创
中医药 (TCM) 是一种古老的个体化医疗形式,可提高食管癌患者的发病率和死亡率。这项回顾性研究旨在评估中医药治疗IV期食管鳞状细胞癌(SCC)的效用。
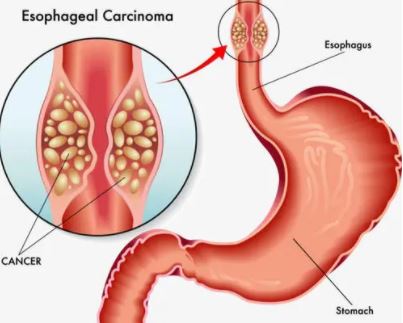
食道癌是一种致命的、但尚未得到充分研究的消化系统恶性肿瘤。其发病率和死亡率分别居世界第 8 位和第 6 位,仅中国就占全球食管癌病例的 50%,2015 年报告的死亡人数为188,000。
许多研究检查了中医药(TCM)在食管癌治疗中的应用。这些报告表明,基于中医的疗法既可以提高西医治疗的疗效并减少西医治疗的副作用,也可以直接诱导肿瘤细胞凋亡。然而,对于基于中医标准的治疗适应症知之甚少,并且缺乏关于晚期食管鳞状细胞癌 (SCC) 患者中基于中医疗法的使用率和结果的可用数据。
与大多数癌症一样,食道癌的护理标准是化学疗法、放射疗法和/或手术的组合。中医治疗依靠“辨证论治”的原则。这个过程包括观察、倾听和询问患者,同时进行基本的身体检查,以便开出最好的治疗方法。正确的辨证论治对中医的疗效至关重要。

方法:收集了 2017 年 7 月至 2020 年 6 月河南省中医院和林州市中医院收治的 IV 期 SCC 患者的病历。使用单变量和多变量分析来确定使用中药是否改善了患者预后. 此外,聚类分析用于根据中医证候类型对患者进行分类,并确定最常用的治疗组合。

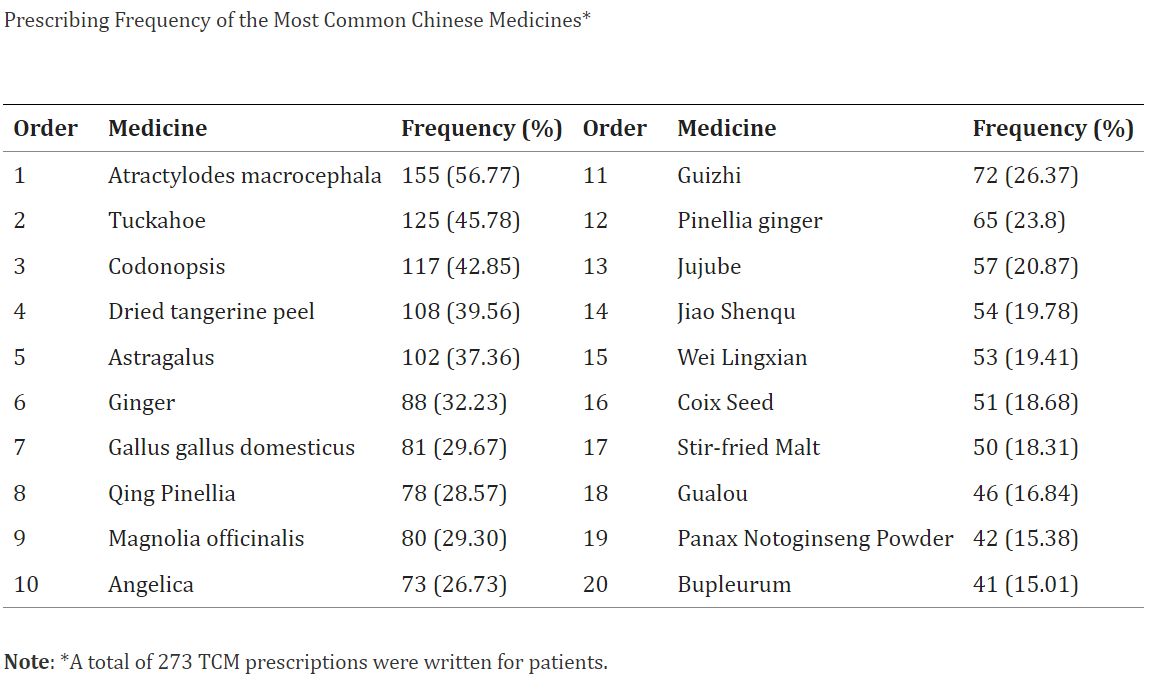
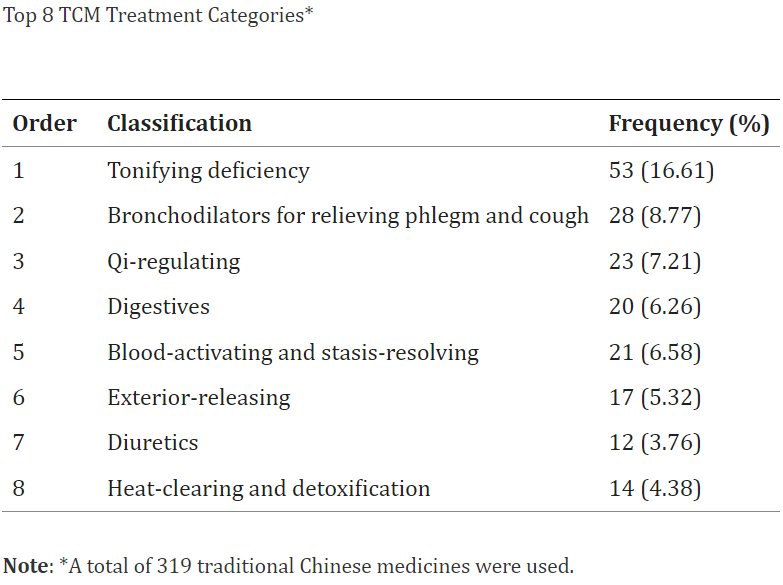
结果:其后402例患者纳入PSM,其中196例(48.8%)接受中药治疗。中医药延长IV期食管鳞癌患者的生存时间(P =0.084),并且与Cox多元回归分析的预后独立相关[风险比(RR)=0.543,95%置信区间(CI):0.390 –0.755,P <0.001]。关联分析显示,75例(38.26%)有痰瘀互结证,53例(27.04%)有痰瘀证,38例(19.39%)有阳气虚证,30例(15.31%)有热量滞留和液体消耗综合征。
结论:中医药衍生疗法治疗可能会增加 IV 期食管 SCC 患者的生存时间。由于这些患者被诊断为不同的中医证候,个体化中医治疗对于改善症状和生存至关重要。
综上所述,这项回顾性队列研究表明,中医药治疗是 IV 期食管 SCC 患者的预后保护因素,并且可能将长期生存期延长两个月。不可否认,无论是辨证论治,还是西医的辅助治疗,中医药对食管癌的治疗都是有用的。基于中医的综合方法可以减少西医治疗的不良反应,提高治疗敏感性,减少复发的机会。在此研究中,“辨证论治”的个体化本质是提高 IV 期 SCC 患者寿命的关键。
原文:Li H, Ma C, Chang S, Xi Y, Shao S, Chen M, Ren J, Sun M, Dong L. Traditional Chinese Medicine Decoctions Improve Longevity Following Diagnosis with Stage IV Esophageal Squamous Cell Carcinoma: A Retrospective Analysis. Int J Gen Med. 2022 Feb 16;15:1665-1675. doi: 10.2147/IJGM.S346536. PMID: 35210836; PMCID: PMC8858954.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#细胞癌#
81
👍🏻👍🏻👍🏻
111
#食管鳞状细胞癌#
110
#食管#
90