BMC Cancer:白蛋白紫杉醇联合PD-1抑制剂信迪利单抗是晚期软组织肉瘤(STS)的有前景治疗方案
2022-01-15 yd2015 MedSci原创
研究表明,白蛋白紫杉醇联合PD-1抑制剂信迪利单抗可作为晚期软组织肉瘤(STS)的有效治疗方案。
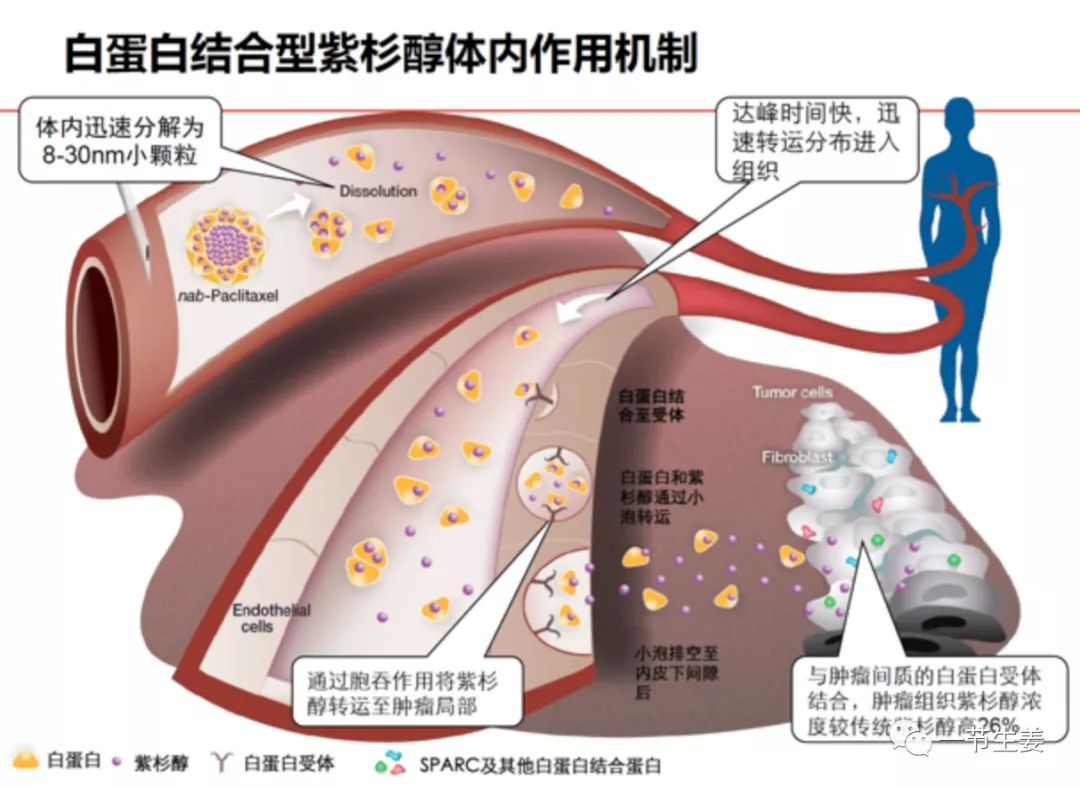
白蛋白紫杉醇联合PD-1抑制剂在多种肿瘤中显示出较好的抗肿瘤活性。但是其在晚期软组织肉瘤(STS)的疗效尚不清楚。因此,来自河南省肿瘤医院团队开展了回顾性研究,评估白蛋白紫杉醇联合PD-1抑制剂信迪利单抗治疗晚期软组织肉瘤(STS)患者的疗效。相关结果发表在BMC Cancer杂志上。
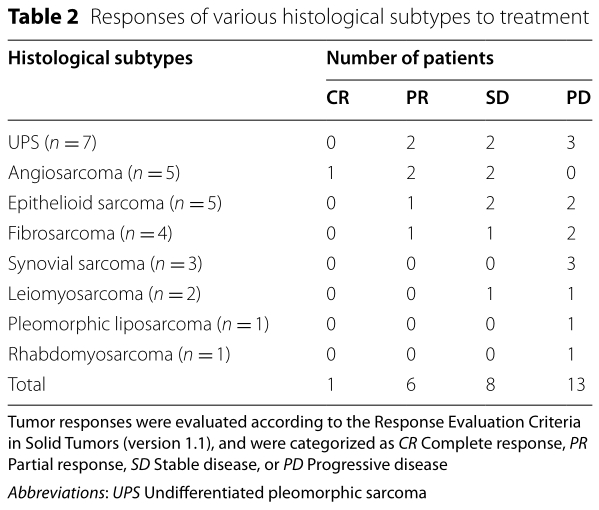
研究纳入28例接受白蛋白紫杉醇联合PD-1抑制剂信迪利单抗治疗的晚期软组织肉瘤(STS),其中女性15例,男性13例。组织学亚型包括未分化多形性肉瘤(7例)、血管肉瘤(5例)、上皮样肉瘤(5例)、纤维肉瘤(4例)、滑膜肉瘤(3例)、平滑肌肉瘤(2例)、多形性脂肪肉瘤(1例)和横纹肌肉瘤(1例)。
在28例晚期STS患者中,1例血管肉瘤患者为CR, 6例为PR, 7例为SD。ORR、DCR、中位无进展生存期(PFS)和4个月无进展生存期率分别为25%、50%和2.25个月(95% CI;1.8 3.0个月),17.9%。

疗效和预后
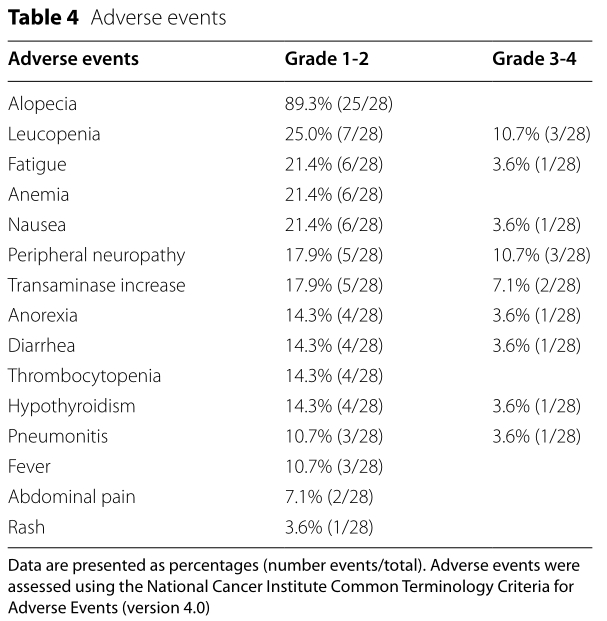
最常见的1级或2级AEs为脱发(89.3%;25/28),白细胞减少症(25.0%;7/28),疲劳(21.4%;6/28),贫血(21.4%;6/28),恶心(21.4%;6/28)。最常见的3级AEs为中性粒细胞减少症(10.7%;3/28)和周围神经病变(10.7%;3/28)。未见4级AEs。所有患者均未因AEs而减少剂量,且未发生治疗相关死亡。
AEs
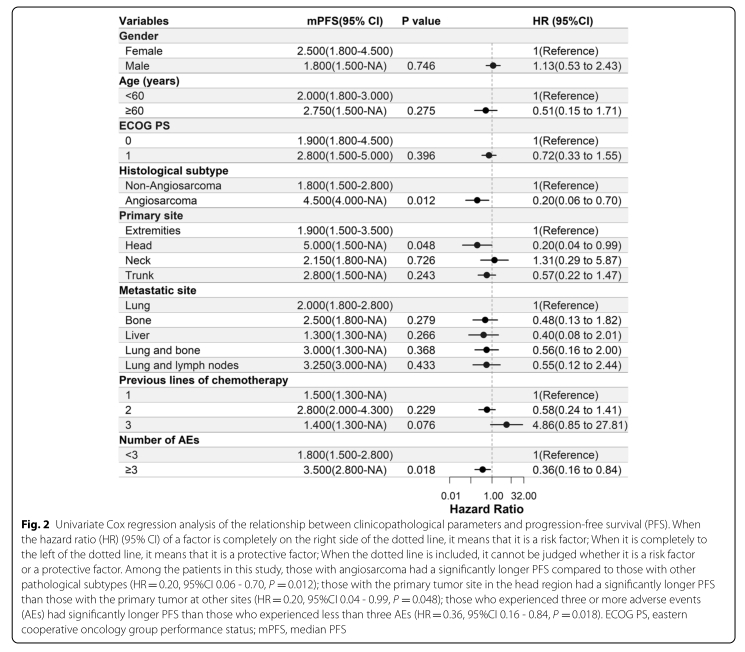
在我们的患者队列中,血管肉瘤患者的PFS明显长于其他病理亚型(HR = 0.20, 95%CI 0.06 - 0.70, P = 0.012);原发部位在头部的患者PFS明显长于其他部位的患者(HR = 0.20, 95%CI 0.04 ~ 0.99, P = 0.048);出现三种及以上AE的患者PFS显著长于三种以下的患者(HR = 0.36, 95%CI 0.16 - 0.84, P = 0.018)。
亚组分析
综上,研究表明,白蛋白紫杉醇联合PD-1抑制剂信迪利单抗可作为晚期软组织肉瘤(STS)的有效治疗方案。
原始出处:
Tian Z, Dong S, Yang Y, Gao S, Yang Y, Yang J, Zhang P, Wang X, Yao W. Nanoparticle albumin-bound paclitaxel and PD-1 inhibitor (sintilimab) combination therapy for soft tissue sarcoma: a retrospective study. BMC Cancer. 2022 Jan 12;22(1):56. doi: 10.1186/s12885-022-09176-1. PMID: 35022029.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#治疗方案#
138
#有前景#
84
#抑制剂#
93
#信迪利单抗#是晚期#软组织肉瘤#的希望
129
#BMC#
76
#PD-1抑制剂#
95
#白蛋白#
82
#软组织#
77
学习#学习#
74