JAMA Netw open:儿童甲状腺结节的分子图谱评价及基因组分类器的应用
2022-06-12 laingying MedSci原创
多基因GC检测具有较高的敏感性和特异性,可增加儿童甲状腺结节的诊断检查,并可能减少诊断性手术的应用。
儿童甲状腺癌的发病率正在上升,目前已成为青少年第二常见的恶性肿瘤。虽然儿童甲状腺结节的发病率低于成人(约2%vs30%),但是恶性风险更高(约25%vs5%)。细针吸取(FNA)细胞学检查是甲状腺结节最常见的诊断方法,但结果往往不确定。
由于肿瘤恶性的可能性很大,目前儿童甲状腺结节的明确诊断是通过诊断性手术获得的,然而,这是有一定风险的,因为儿童甲状腺手术与较高的并发症发生率相关。在成人中,术前分子检测可改善甲状腺结节的治疗,但在儿童中尚未得到验证。
本研究的目的是确定儿童甲状腺结节的分子形态是否可通过多基因基因组分类器(GC)检测。
这是一项连续的回顾性病例分析系列,对2003年1月至2019年12月在某三级学术医疗中心进行的儿童甲状腺连续切除术中细针穿刺(FNA)和福尔马林固定石蜡包埋(FFPE)组织进行GC检测。该研究包括95例患者(中位年龄16.3岁[4.8 - 21.1],其中75例[79%]女性)因甲状腺结节接受手术。总共118个甲状腺结节样本(95个FFPE,23个伴生FNA)产生了信息丰富的下一代测序数据和多基因GC。
主要结局是确定儿童甲状腺分子结构,次要结局是探讨小儿甲状腺结节的GC检查诊断的准确性。
结果显示,下一代测序证实了儿童恶性甲状腺结节(与成人相比)的独特分子格局,主要由基因融合(最常见的是RET和NTRK)、罕见的BRAF/RAS改变、无TP53或TERT启动子致病性突变体构成。一些低分化甲状腺癌含有DICER1变体。良性结节几乎完全与TSHR和DICER1改变相关。该试验的敏感性为96%(95%CI,87%~99%),特异性为78%(95%CI,64%~88%)。阴性预测值为95%(95%CI,88%~98%),阳性预测值为83%(95%CI,74%~89%)。23对匹配的FFPE和FNA组织的GC一致性为96%。
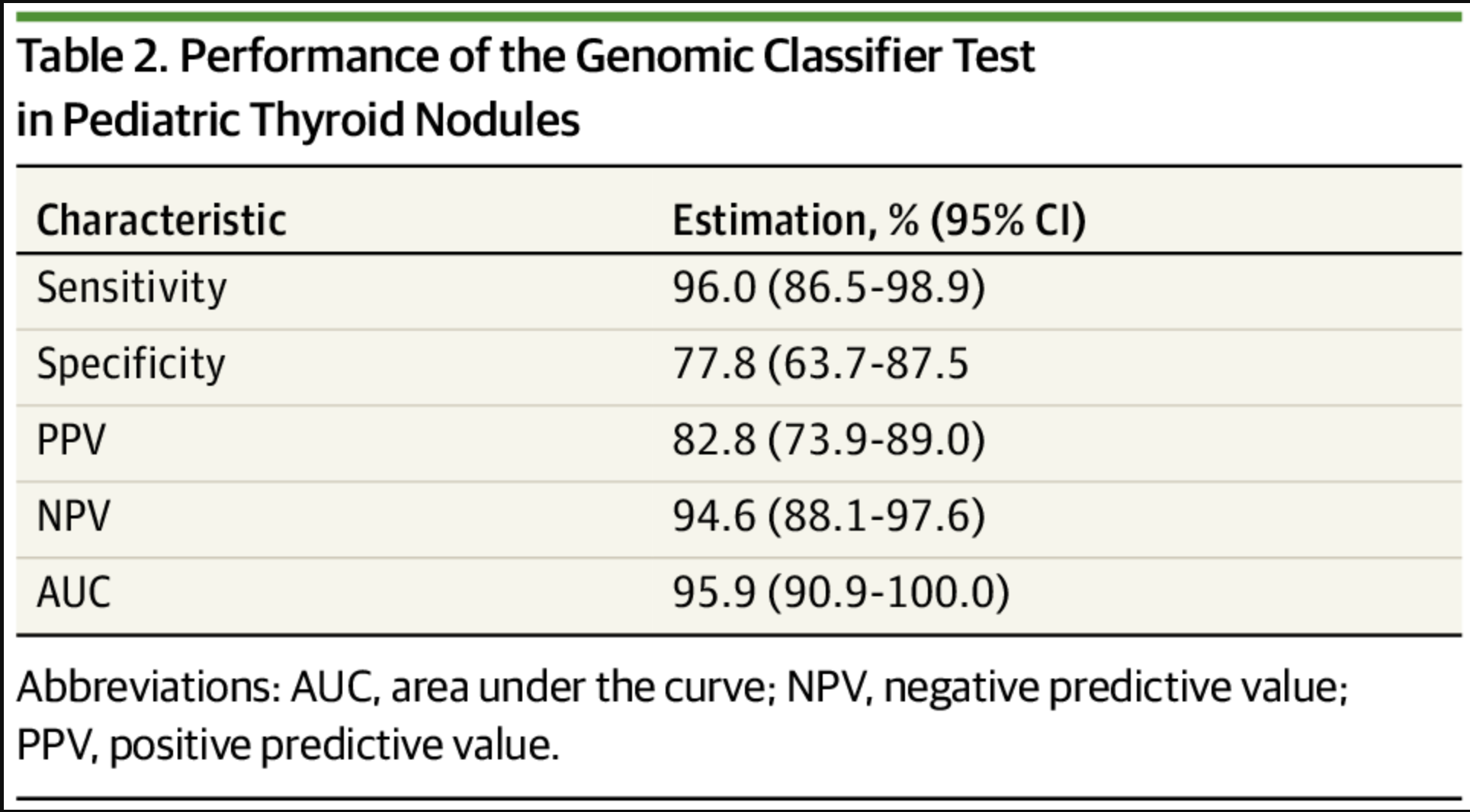
基因组分类器检测在儿童甲状腺结节中的应用
简单来说,这一连续的回顾性病例研究结果表明,儿童甲状腺结节的分子结构的确是独特的,但仍可进行进一步的子分类。多基因GC检测具有较高的敏感性和特异性,可增加儿童甲状腺结节的诊断检查,并可能减少诊断性手术的应用。
参考文献:Gallant J, Chen S, Ortega CA, et al. Evaluation of the Molecular Landscape of Pediatric Thyroid Nodules and Use of a Multigene Genomic Classifier in Children. JAMA Oncol. Published online June 09, 2022. doi:10.1001/jamaoncol.2022.1655
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#NET#
60
#PE#
49
#分子图谱#
56
#评价#
78
JAMA上文章都是顶级的,谢谢梅斯及时上新
64