游离股前外侧皮瓣修复大面积颈枕部头皮缺损1例
2019-10-28 不详 临床骨科杂志
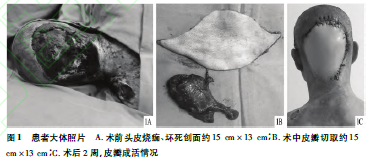
患者,男,38岁,因高压电击伤致意识不清2h,在当地县医院急诊予气管插管、呼吸机应用后转入我院继续治疗。查体:神志模糊,持续气管插管,呼吸机应用,双侧瞳孔直径约0.2cm,对光反应存在,腹平软,肝脾肋下未及,枕部及后颈部见约15cm×13cm头皮烧痂、缺损,局部颅骨外露伴渗出,见图1A。经我院ICU积极治疗后患者神志转清、病情转平稳,于2018年2月4日转我科进一步手术治疗。于2018年2月6日、
临床资料
患者,男,38岁,因高压电击伤致意识不清2h,在当地县医院急诊予气管插管、呼吸机应用后转入我院继续治疗。查体:神志模糊,持续气管插管,呼吸机应用,双侧瞳孔直径约0.2cm,对光反应存在,腹平软,肝脾肋下未及,枕部及后颈部见约15cm×13cm头皮烧痂、缺损,局部颅骨外露伴渗出,见图1A。经我院ICU积极治疗后患者神志转清、病情转平稳,于2018年2月4日转我科进一步手术治疗。于2018年2月6日、14日、21日分别行清创+负压封闭引流术,术后创面转新鲜,于2018年2月26日在全身麻醉下行颈枕部清创+游离股前外侧皮瓣修复术。术中采用右侧卧位,术中切取股前外侧皮瓣约15cm×13cm(见图1B),将旋股外侧动脉降支与左侧颞浅动脉吻合,相应伴行静脉予以吻合。手术顺利,术后皮瓣成活,供区直接缝合、创口愈合良好,见图1C。于2018年3月12日出院。术后随访9个月,皮瓣成活良好。
讨论
本例患者头皮缺损面积大,常规行局部皮瓣转移则不能完全覆盖创面,还需部分皮片移植;行头皮扩张则需要长时间注水扩张、不宜早期修复;而旋股外侧动脉降支与颞浅动脉管径大小基本吻合,故游离股前外侧皮瓣转移可一期修复缺损创面、供区隐蔽可直接缝合。本例手术方式对大面积头皮早期缺损的患者具有一定的借鉴意义,但对后期皮瓣无发区要求美容者,建议整形美容科行头皮扩张术更加完美。
原始出处:
万绍乐,沈永辉,季卫平.游离股前外侧皮瓣修复大面积颈枕部头皮缺损1例[J/OL].临床骨科杂志,2019(05):573[2019-10-28].
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#大面积#
0
#颈枕部#
63
#皮瓣#
75