Blood:原发性渗出性淋巴瘤!
2018-08-30 MedSci MedSci原创
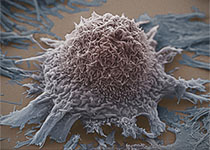
原发性渗出性淋巴瘤(PEL)是一种罕见的B细胞恶性肿瘤,主要发生于免疫功能不全的患者,如HIV感染者和进行器官移植的患者。PEL的主要特征是恶性渗出,表现为浆膜腔积液,一般无肿瘤包块。其发病与8型人疱疹病毒/卡波西肉瘤相关疱疹病毒潜伏感染相关,肿瘤细胞的正常对应细胞为向浆细胞分化的B细胞。免疫缺陷和缺乏CD20表达导致抗CD20单克隆抗体缺乏预期的疗效;PEL的临床预后极其不良,1年总体存活率仅3
其发病与8型人疱疹病毒/卡波西肉瘤相关疱疹病毒潜伏感染相关,肿瘤细胞的正常对应细胞为向浆细胞分化的B细胞。免疫缺陷和缺乏CD20表达导致抗CD20单克隆抗体缺乏预期的疗效;PEL的临床预后极其不良,1年总体存活率仅30%。
尽管抗逆转录病毒疗法的进展改善了HIV感染患者的预后,但对于PEL患者,预后仍未得到明显改善。此外,肿瘤细胞一般高表达PDL1,一种重要的免疫检查点分子,可导致肿瘤细胞逃脱宿主免疫防御,这可能是PEL治疗效果差的潜在机制。针对PEL的激活的信号通路的分子靶向疗法,如NF-κB、JAK/STAT和PI3K/AKT,已开始应用于治疗PEL。
将免疫缺陷恢复、克服免疫逃逸和开发更为有效的药物三者结合起来,对提高PEL患者的预后至关重要。
原始出处:
Kazuyuki Shimada, Fumihiko Hayakawa, and Hitoshi Kiyoi. Biology and management of primary effusion lymphoma. Blood 2018 :blood-2018-03-791426; doi: https://doi.org/10.1182/blood-2018-03-791426
本文系梅斯医学(MedSci)原创编译,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#原发性渗出性淋巴瘤#
62
#原发性#
68
学习了
116