香港著名影星吴孟达因肝癌去世,享年70岁
2021-02-27 JACKZHAO MedSci原创
据香港媒体报道,吴孟达(达哥)今日(27/2)因肝癌于仁安医院逝世,终年70岁。早前已不断传出达哥病危的消息,好友田启文(田鸡)早前向传媒透露达哥不幸罹患肝癌,两个月前已做过切除手术,不过身体尚未复原

据香港媒体报道,吴孟达(达哥)今日(27/2)因肝癌于仁安医院逝世,终年70岁。早前已不断传出达哥病危的消息,好友田启文(田鸡)早前向传媒透露达哥不幸罹患肝癌,两个月前已做过切除手术,不过身体尚未复原,要接受化疗。
田启文接受媒体采访称香港著名影星吴孟达因肝癌去世,享年70岁。下午17时19分,田启文在医院门口接受媒体采访,称吴孟达已经在2分钟前离开了大家,“大哥是以睡觉的姿态离开的,走的时候非常安心。”
2月27日早些时候,港媒突传70岁吴孟达病危,已经转入ICU抢救,医生已经通知亲友见最后一面。
报道称,吴孟达在两个月前做手术,因为扩散要接受化疗,好友田启文表示达哥第三任太太马来西亚籍侯珊燕已从马来西亚赶来,因为疫情,要完成隔离后才可到医院陪他;至于她为达哥生下的一对子女在国外读书,正安排他们到港探望父亲。有媒体此前报道,吴孟达曾透露,为了防止以后突然有什么状况发生,已悄悄立下遗嘱。
吴孟达先后有三段婚姻,前两任太太为他生了3个女儿,跟现任太太侯珊燕于1996年结婚,育有1子1女。侯珊燕曾获马来西亚小姐季军并加入娱乐圈,于1993年在新加坡拍电影《花田囍事》时跟达哥合作并结下情缘,1996年奉女成婚,2003年添第一个儿子。达哥曾表示要照顾3个家庭、5名子女,负担很重,故一直努力工作。

吴孟达(英语:Ng Man-tat,1951年1月2日-2021年2月27日),生于福建省厦门市,香港男演员,与周星驰合作多套喜剧片。也曾获得多届香港电影金像奖和台湾电影金马奖最佳男配角提名,并以《天若有情》荣获第10届香港电影金像奖最佳男配角。
吴孟达生前代表作有《楚留香传奇》《天若有情》《逃学威龙》《破坏之王》《九品芝麻官》《武状元苏乞儿》《食神》《少林足球》《流浪地球》等。
近年来,很多耳熟能详的明星都是因为肝癌离世的。
近年2月3日,年仅43岁的知名音乐人、演员赵英俊因肝癌病逝;
2019年,69岁的香港演员李兆基因肝癌扩散至肺部去世;
2018年9月28日,54岁的歌手臧天朔因肝癌去世;
就在同一天晚间,66岁的相声表演艺术家师胜杰也因肝癌病逝;
2005年,42岁演员傅彪因肝癌去世。
据世界卫生组织国际癌症研究机构(IARC)发布的 2020 年最新全球癌症负担数据显示:2020 年我国肝癌死亡病例数达 39 万例,仅次于肺癌排在第二位。

2018年全球肝癌发病率与死亡率情况,肝癌流行趋势与分析
中国肿瘤登记地区肝癌男女发病比为3.0左右(范围是2.64~3.54),20年比值变化差异无统计学意义(P=0.150);肝癌的城乡发病比值由1989年的0.51上升到2008年的0.61(P<0.01)。1989年男性肝癌平均发病年龄为57.14岁,女性为61.69岁,2008年男性肝癌平均发病年龄为60.34岁,女性为66.47岁,20年间肝癌平均发病年龄升高(P<0.01)。这表明中国1989–2008年肝癌发病率男女差异变化不明显,城乡差异在缩小,平均发病年龄在后移。
然而,四川大学华西公共卫生学院流行病学研究指出,2015年中国恶性肿瘤标化死亡率为159.01/10万,≥70岁 人群死亡率最高(1 102.73/10万),5—14岁年龄组死亡率最低(5.40/10万),男性标化死亡率是女性的2.15倍,死亡率最高的5个省份分别是安徽、青海、四川、广西和河南,以肺癌、肝癌、胃癌、食道癌和结直肠癌死亡率最高。
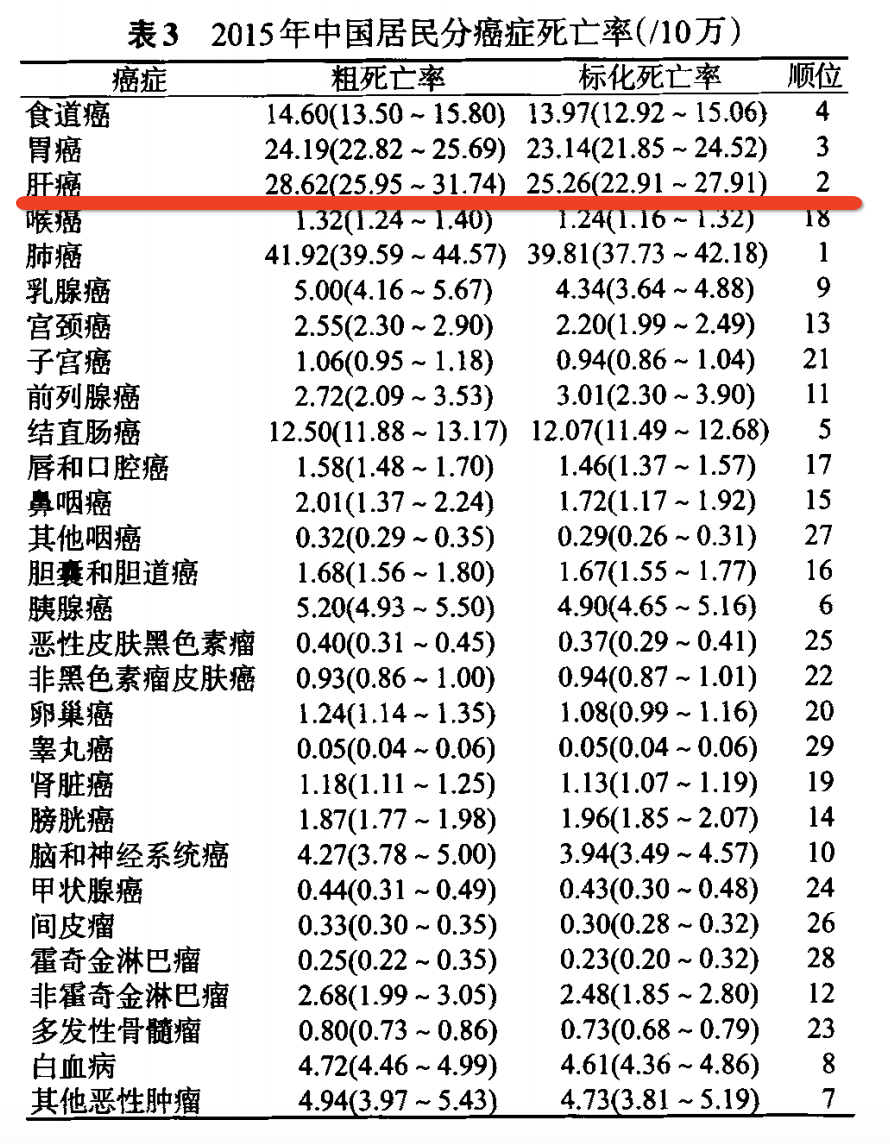 中国居民2015年恶性肿瘤死亡率流行病学特征分析,四川大学华西公共卫生学院流行病与卫生统计学系
中国居民2015年恶性肿瘤死亡率流行病学特征分析,四川大学华西公共卫生学院流行病与卫生统计学系
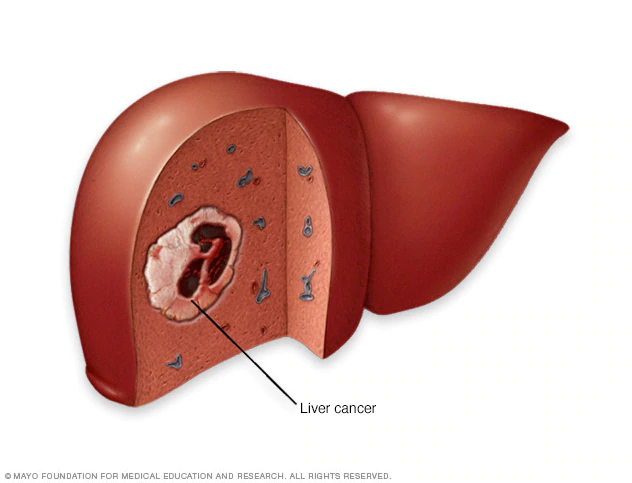
肝癌主要分为原发性肝癌、转移性肝癌两大类,两者的性质也是截然不同。原发性肝癌(primary liver cancer)是指原发于肝细胞或胆管细胞的癌症,大多数肝癌皆属肝细胞癌,所以通常称为肝癌,唯有少部分发生在肝内的胆小管,称为胆管细胞癌。继发性或转移性肝癌(secondary liver cancer):癌细胞最初发生在其他部位,最后转移至肝脏。因肝脏血管构造丰富,癌细胞可经由血液入侵。大多数肝癌都是继发性或转移性的。
肝癌患者以男性居多,原发性肝癌的主要成因包括:肝硬化,慢性病毒性肝炎,其中慢性乙型肝炎是最常见的原因,服用某些有毒的化学物质(如发霉花生或其他食品产生的黄曲霉毒素),长期酗酒,长期受到某些环境污染物侵害(如吸入制胶厂使用的聚氯乙烯)。
肝癌的常见征状
早期肝癌一般没有任何病征,其后出现的征状包括:
右上腹疼痛
发烧
皮肤及眼睛泛黄
腹部肿胀
小便呈茶色而大便呈浅灰色
食欲不振
恶心
体重下降
疲倦及虚弱
我们在惋惜的同时,不妨也将目光移到 " 罪魁祸首 " 肝癌上来看一看,到底它为何可以轻易夺去一个个生命?
1. 缺乏有效的早期筛查
据统计,肝癌早期的发现率不足 15%,绝大多数患者在被发现时已到中晚期。
由于肝脏本身没有痛觉神经,出现问题时很难迅速察觉。因此,想要尽早发现肝部的异常,除定期体检筛查外,还需要进行肝功、肝胆系统彩超的检查。
2. 肝炎病毒感染
乙肝病毒和丙肝病毒感染是我国肝癌发生的常见危险因素。如果在感染病毒后不及时救治,就有很大风险转为肝纤维化、肝硬化,进而形成肝癌。
3. 不良的生活习惯
加班、玩游戏、看剧 …… 总有理由让我们在深夜迟迟无法入眠。" 一时熬夜一时爽,一直熬夜一直爽 "。熬夜成为癌症以及其他多种疾病的诱因。
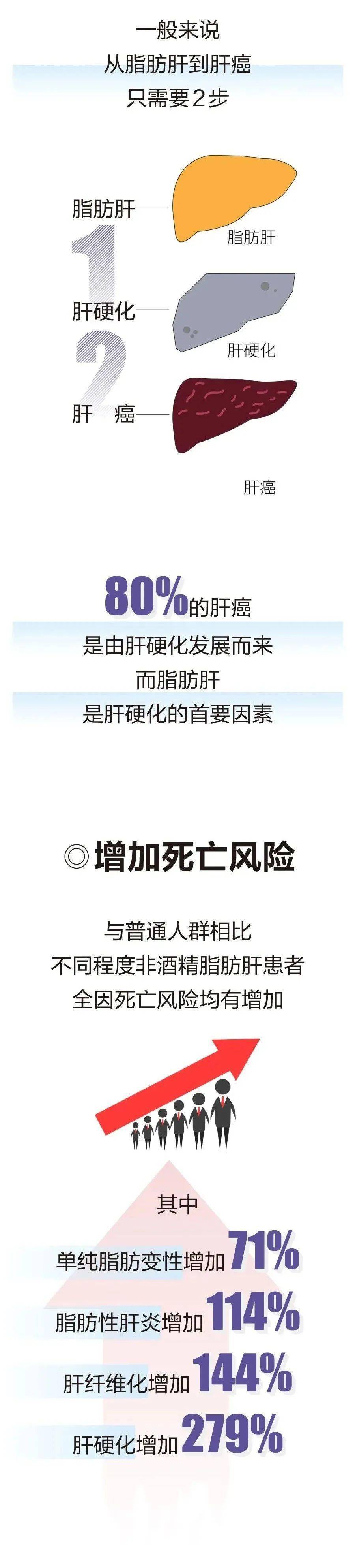
2016 年,一项发布于《癌细胞》杂志上的研究发现:将小鼠暴露于不规律的昼夜周期近 2 年,小鼠体重增加并发展为脂肪肝,在某些情况下会发展为慢性炎症,并最终发展为肝癌。
除熬夜外,饮酒也是肝脏 " 杀手 " 之一。据英国一项研究统计,约 30% 的酒精性肝硬化患者会发展为肝癌。
此外,高油、高糖、高盐的饮食,不规律、不健康的饮食等不良生活习惯同样会给肝脏带来巨大负担。
护肝的六大饮食原则:
口味清淡,避免加工食物
避免食用腌渍、烟熏等加工食物,也避免摄取过多盐分,造成身体负担。
蔬果饮食,选择高纤食物
多食用富含维生素 B、C 的黄绿色蔬菜及水果,增加身体抗氧化能力。可增加全谷类食材,增加纤维质摄取、避免便秘。
足够热量,摄取蛋白质
选择蛋、豆、鱼、肉类等食材补充蛋白质,且应增加热量的摄取,以理想体重每公斤40卡的热量为准。若有肝昏迷现象,则应减少蛋白质摄取量,亦可请教营养师适合的饮食方式。
少量多餐,增加进食量
治疗期间或术后若有食欲不佳的情况,可采用少量多餐的方式,每天6-8餐,维持营养、热量补充。
戒烟戒酒
吸烟及酒精都会加重肝脏的负担,唯有戒烟戒酒才能提供肝脏健康的恢复状态。
勿信偏方
均衡饮食是摄取足够营养的正确方式,切勿相信偏方、私自服用草药、不明药物等,否则可能延误治疗、加重病情。
肝癌的疗法主要与癌症属于原发性或继发性而定,患者可能需要接受外科手术、化疗(使用抗癌药物)、放射治疗(利用X光对付或消灭癌细胞)或混合以上多种治疗法,部份肝癌患者可接受肝脏移植。至于哪种才是最适当的疗法,则要视乎病情的严重性、肝癌对患者生活的影响程度,以及是否有其他病态出现而定。
最后一点,最为重要的是的:癌症最好的治疗就是预防,早发现早治疗,如果你怀疑自己有肝癌,必须及早就医。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













防大于治
91
达叔走好 #吴孟达#
141
#去世#
83
早睡 避免熬夜
125
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
0
不错
1
不错
104
致敬一个时代致敬一个时代
100
遗憾
81