Nutrients:益生元研究的新近进展 —— 专家研讨会声明
2018-02-17 张灵 | 消化客 江苏省人民医院消化科
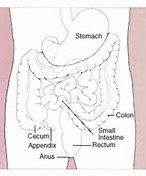
人类肠道微生物群由1013-1014个微生物组成(主要是细菌),其参与多种生物过程,如营养物质的利用和能量储存、抗感染、免疫系统的成熟和功能调节、支持神经内分泌功能等,因此,对整体健康状况至关重要。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#研讨会#
59
谢谢分享.
106
益生元研究的治疗.
71
学习了
85
学习了.谢谢分享
94
益生元研究的进展.
77
学习学习
61
学习了
63
学习了
55
#益生元#
75