Pembrolizumab在罕见组织肉瘤中提供临床益处!
2020-09-21 Allan MedSci原创
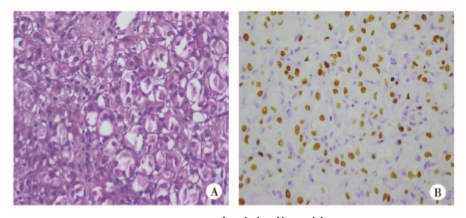
II期AcSéPembrolizumab临床试验评估了Pembrolizumab单一疗法治疗罕见肉瘤的有效性和安全性。
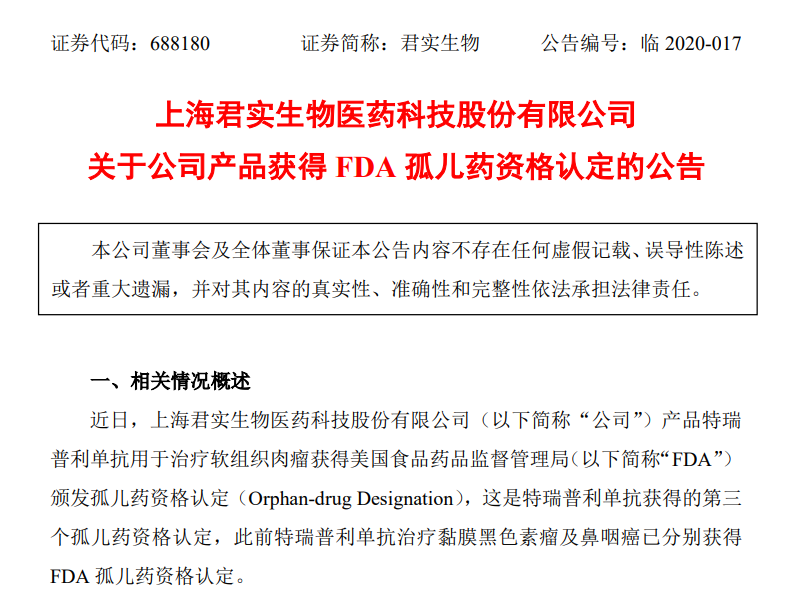
II期AcSéPembrolizumab临床试验评估了Pembrolizumab单一疗法治疗罕见肉瘤的有效性和安全性,结果显示,不同组织类型的肉瘤患者的无进展生存期(PFS)和总体生存期(OS)有所不同。这项研究近期发表于2020年ESMO虚拟大会之上。

AcSéPembrolizumab研究是一项非随机、平行臂、开放标签、多中心II期临床试验,所评估的组织型均为罕见肉瘤,每年发病率低于0.2例/100,000人。纳入标准:患者年龄>18岁,ECOG≤1,且对标准疗法有抵抗力的晚期疾病患者。Pembrolizumab以200 mg静脉内给药,在每21天周期的第1天输注30分钟。该研究的主要终点是客观缓解率(ORR)。次要终点包括临床受益率(CBR)、反应持续时间(DoR)、PFS、OS和安全性。
将80例罕见肉瘤患者按组织学类型分为5组:脊索瘤(n = 24)、肺泡软部肉瘤(ASPS,n = 13)、增生性小圆形细胞瘤(DSRCT,n = 6)、Smarca4缺失的恶性横纹肌瘤(SMBT,n = 6)和其他组织型(n = 31)。结果显示,在脊索瘤中,中位PFS为5.7个月;在ASPS中,中位PFS为14个月;在DSCRCT中,中位PFS为5个月;在SMBT中,中位PFS为未达到;在其他组织学类型中,中位PFS为2.7个月(p = 0.00016)。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Pembro#
69
#PE#
87
#mAb#
94
#肉瘤#的#免疫治疗#,以及#放疗#,#抗血管新生治疗#,都是选择
313
#Pembrolizumab#
89
#罕见#
72