Carcinogenesis:研究发现胰腺癌的新型治疗靶点
2019-05-07 佚名 上海营养与健康研究所
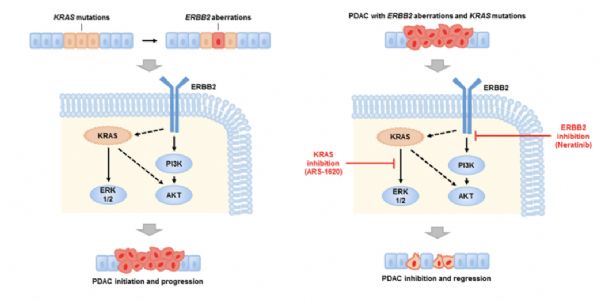
5月2日,国际肿瘤学学术期刊Carcinogenesis 在线发表了中国科学院上海营养与健康研究所-长征医院联合转化医学中心王跃祥研究组题为Oncogenic ERBB2 Aberrations and KRAS Mutations Cooperate to Promote Pancreatic Ductal Adenocarcinoma Progression 的转化医学研究成果,该研究揭示了
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#治疗靶点#
60
#Carcinogenesis#
71
#研究发现#
51
#CIN#
51
#Gene#
69
#ESI#
55