衰老是一种细胞周期停滞的状态,在胚胎发生、伤口愈合和预防癌症中起着重要作用。衰老的关键驱动因素为衰老细胞(senescent cell)。衰老细胞具有“促生存网络” ,可以抵抗细胞凋亡或程序性细胞死亡,因此会随着机体衰老而累积。它们释放一系列促凋亡、促炎、导致干细胞功能紊乱、破坏组织、向正常细胞扩散衰老、衰老相关分泌表型(SASP)的因素。这导致了与年龄相关的疾病和慢性疾病的发生,如动脉粥样硬化、2型糖尿病、关节炎、特发性肺纤维化和肝病。

图片来源:摄图网
2015年,美国梅奥医学中心的James Kirkland博士在Aging Cell发表的论文中,首次提出Senolytics(抗衰老药物)一词,特指选择性杀伤衰老细胞的药物。抗衰老药物,如达沙替尼、槲皮素和非西汀,在动物模型中产生健康益处并延长寿命。因此,如果在人类身上是安全有效的,抗衰老药物将有希望助老年人延迟、预防或治疗多年龄和慢性疾病相关疾病。
虽然抗衰老药物能够延缓或减轻许多与年龄相关的疾病,但很明显,抗衰老药物并不能杀死所有的衰老细胞。因此,确认哪些衰老细胞类型最有可能驱动衰老,并以之作为最重要的治疗靶点,仍然是一个关键的问题。
衰老与免疫衰老
在衰老的过程中,免疫系统会失去对抗病原体和癌细胞的有效反应能力,即免疫衰老。其特征为未致敏T细胞: 记忆T细胞比率、CD4:CD8比率、钙介导信号受损和胸腺萎缩等。这些变化限制了接种疫苗的有效性,增加了疾病易感性,并导致老年人死亡。然而,对于老年免疫系统如何导致免疫衰老这个问题,科学界却知之甚少。
2021年5月12,美国明尼苏达大学的两位教授Paul Robbins和Laura Niedernhofer联合通信,于 Nature在线发布了名为 “An Aged Immune System Drives Senescence and Ageing of Solid Organs” 的研究论文,结果表明衰老的免疫细胞会导致全身组织损伤,缩短寿命。
图片来源:Nature官网
这项研究的主要结论是内源性DNA损伤容易影响免疫细胞,若不修复,就会导致细胞死亡或衰老,因此衰老的免疫细胞也成为延长健康寿命的关键治疗靶标。与正常衰老一样,实验室中的衰老损害先天免疫和适应性免疫——特别损害滤泡辅助性T细胞和自然杀伤细胞的功能,并潜在地驱动身体器官的衰老。实质损伤的机制似乎是细胞自主性(功能丧失)和细胞非自主性(功能获得,如SASP)的结合。研究人员总结,利用抗衰老药物靶向治疗衰老免疫细胞,在抑制多种老年疾病方面十分具有潜力。
在实验小鼠中,减少内切酶ERCC1-XPF的表达会破坏DNA的损伤修复,并在多种组织中加速内源性氧化损伤和衰老细胞的积聚。这导致一系列与衰老相关的早发性疾病与组织病理学。因此,团队在小鼠造血细胞中选择性删除了ERCC1基因,仅在免疫系统中增加内源性DNA损伤的负担,从而导致免疫细胞衰老。
许多免疫细胞随着年龄的增长而衰老,其p16和p21的表达水平增加,同时表达一种衰老相关泌表型(SASP)。通过检测细胞衰老标志物(p16和p21)以及SASP,实验发现变异小鼠的B细胞、T细胞、自然杀伤细胞和巨噬细胞中的p16和p21明显升高。SASP在T细胞、自然杀伤细胞和巨噬细胞中的表达同样增加。这表明缺失ERCC1所增加的内源性DNA损伤可导致免疫细胞衰老。
研究发现,变异小鼠的特异性免疫细胞群损耗和衰老相较于野生小鼠更为严重。在衰老过程中,野生小鼠的淋巴细胞计数稳定,而变异小鼠的B细胞(B220+CR19+)和T细胞(CD4+和CD8+)均显著减少。此外,相较于正常小鼠,变异小鼠的进行性外周白细胞减少,老年变异小鼠的脾脏中T细胞、骨髓中B细胞比例减少。值得注意的是,五个月大的变异小鼠的免疫细胞数量显著减少,并且随着小鼠衰老,细胞数量继续下降,比正常小鼠下降更快。但在衰老过程中,变异小鼠与野生小鼠的变化相似。这表明造血细胞中ERCC1缺失的小鼠健康进入成年期后,免疫系统加速磨损,免疫衰老过早发生。此变化类似于野生型小鼠在衰老过程中发生的变化。
变异小鼠的先天性和适应性免疫功能皆受损。变异小鼠与野生老年小鼠相似的是,足垫肿胀程度减少,抗KLH抗体的血清水平降低。这证明变异小鼠的细胞免疫和体液免疫功能均受到损害。作为健康免疫衰老的生物标志物,自然杀伤细胞介导的细胞毒性可以未经致敏就杀伤靶细胞。然而此能力在变异小鼠中同样减弱。
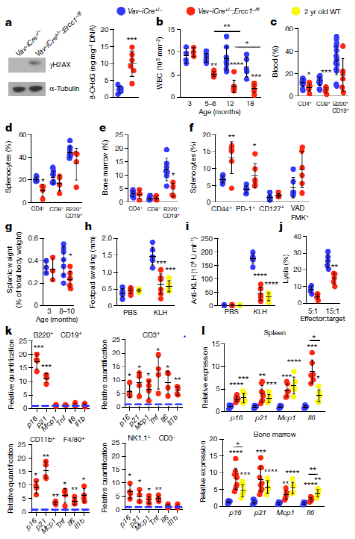
造血细胞中删除ERCC1基因造成免疫系统的加速老化
多处组织中的细胞衰老标志物在老年变异小鼠中表达有所增加,但在年轻变异小鼠表达却不明显。这证明免疫衰老优先于外周衰老。研究发现,免疫器官的衰老和氧化应激反应足以造成正常器官的组织损伤,变异小鼠具体体现为:胰腺功能障碍标志物增加、肝和肾的损害标志物增加、提前呈现椎间盘退行性变的特征、肌肉损伤的再生功能受损、握力降低和寿命降低。因此,非淋巴器官和组织显示严重的衰老和损伤;证明衰老的免疫系统驱动全身的系统性衰老。
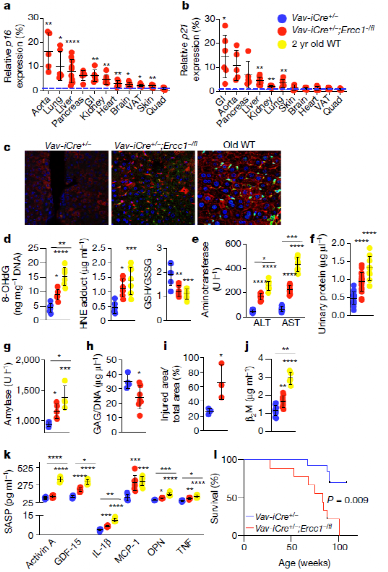
衰老的免疫系统驱动非淋巴器官的衰老和组织稳态的丧失
值得注意的是,研究人员将变异小鼠或老年野生型小鼠的脾细胞移植到野生年轻小鼠,发现被移植野生小鼠衰老加速,寿命显著缩短。反之,若将年轻野生小鼠的脾细胞移植到变异小鼠体内,发现被移植变异小鼠的组织衰老有所减缓。证明衰老的免疫细胞可以通过功能获得机制,即加速组织细胞的非自主衰老,但衰老的免疫细胞也具有功能丧失机制,即无法抑制衰老。
研究人员用雷帕霉素(rapamune)治疗变异小鼠,后测定小鼠免疫功能。结果发现,雷帕霉素降低了外周T细胞中衰老标记物,使抗KLH血清浓度和白细胞计数增加。说明治疗后,小鼠免疫功能提高,免疫衰老有所好转。这证明免疫衰老可以被调节,且免疫衰老可以驱动全身性衰老。
最后,该研究的通讯作者 Laura Niedernhofer 教授表示:“既然我们已经确定了哪种细胞类型是最有害的,这项工作将引导我们开发靶向衰老免疫细胞的衰老解药。我们还希望它能帮助指导免疫细胞群中的生物标记物的发现,帮助判断哪些人有组织损伤和快速老化的风险,从而判断哪些人最需要衰老治疗。”
参考信息
1.Martel, J. et al. Emerging use of senolytics and senomorphics against aging and chronic diseases. Medical Research Reviews. 2020. doi.org/10.1002/med.21702
2.Zhu, Y.et al. The Achilles' heel of senescent cells: from transcriptome to senolytic drugs. Aging Cell. 2015;14(4):644-658. doi:10.1111/acel.12344
3.Matthew, J. Y. et al. An aged immune system drives senescence and ageing of solid organs. Nature. 2021. doi.org/10.1038/s41586-021-03547-7
4.Lagoumtzi, S. M. & Chondrogianni, N. Senolytics and Senomorphics: natural and synthetic therapeutics in the treatment of aging and chronic diseases. Free Radical Biology and Medicine. 2021. doi.org/10.1016/j.freeradbiomed.2021.05.003
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#科学家发现#
75
受益
80
学习
179
受益,不错的选择
97
学习
147
👍🏻
98
有用
110
有帮助
59