ACS Central Science 大肠杆菌又立下新功劳:可用于检测内分泌干扰物
2017-01-16 佚名 生物谷
研究已经表明内分泌干扰物(EDCs)与肥胖、糖尿病及癌症等疾病的发生发展有关,但是研究人员发现包括杀虫剂、塑料及药物等的一系列产品中均含有EDCs。EDCs在低浓度时就有毒副作用,甚至有研究发现游泳池中毫克级别的EDCs都对身体有伤害。现在,研究人员在《ACS Central Science》上发表文章宣布他们可以使用工程化大肠杆菌快速检测出环境中极低浓度的EDCs。 检测EDCs是

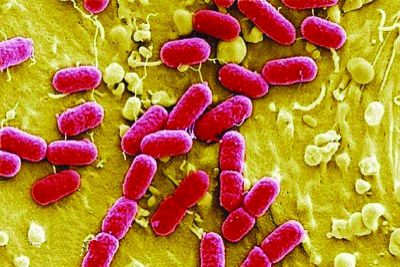
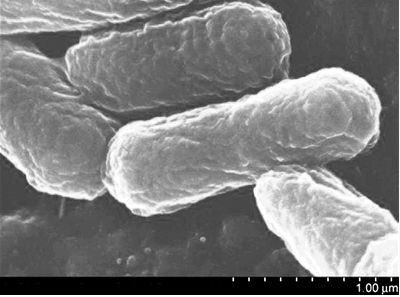
研究已经表明内分泌干扰物(EDCs)与肥胖、糖尿病及癌症等疾病的发生发展有关,但是研究人员发现包括杀虫剂、塑料及药物等的一系列产品中均含有EDCs。EDCs在低浓度时就有毒副作用,甚至有研究发现游泳池中毫克级别的EDCs都对身体有伤害。现在,研究人员在《ACS Central Science》上发表文章宣布他们可以使用工程化大肠杆菌快速检测出环境中极低浓度的EDCs。
检测EDCs是一件非常困难的事情,因为它们是根据活性(即作用的受体种类)来分类,而不是根据结构分类。因此EDCs包含了极其大量的化学物质,而通常健康风险是由于同时暴露在几种EDCs中导致。由于许多EDCs作用于细胞表面相同的受体,因此研究人员已经开发出可以根据它们干扰荷尔蒙的方式进行检测的方法,但是这些方法花费的时间很长,或者涉及复杂而昂贵的检测,使用不方便。
而在这项新研究中,Matthew Francis及其同事在他们的设备中使用了大肠杆菌,成功地解决了这些问题。在他们开发的便携式传感器中含有死亡无毒的大肠杆菌,它们在传感器表面暴露出雌激素受体。传感器表面有一种可以识别EDC-大肠杆菌复合物的蛋白,一旦复合物产生并被蛋白识别,传感器就可以在数分钟内产生电信号并生成相应检测结果。这种便宜的传感器不仅可以检测出许多已知EDCs单独存在时的浓度,还可以检测出不同EDCs组成的混合物的总浓度。
此外,研究人员发现这种传感器可以检测出水溶液以及婴幼儿奶粉复合物溶液中的EDCs种类及含量,还可以检测出塑料婴儿奶瓶在微波加热下释放到液体中的微量EDCs。研究人员声称他们的检测方法还适合在野外使用,可以通过修饰检测许多其他作用于人体受体的化学物质。
原始出处
Ariel L. Furst, Alexander C. Hoepker, Matthew B. Francis.Quantifying Hormone Disruptors with an Engineered Bacterial Biosensor.ACS Central Science, 2017;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TRA#
56
#干扰物#
59
#分泌#
61
#central#
53
#ACS#
66
#大肠杆菌#
52
#SCIE#
40