阿司匹林或将癌症患者的死亡风险降低 20%
2021-07-05 K.K MedSci原创
在对约 250,000 名癌症患者(包含18种癌症)的治疗方案中服用阿司匹林,死亡风险降低 20%
1974 年,威尔士医学研究委员会 Elwood 教授和 Archie Cochrane 教授领导的研究小组首次表明,每天服用一片阿司匹林可使心脏病和中风的死亡率降低约 24%。
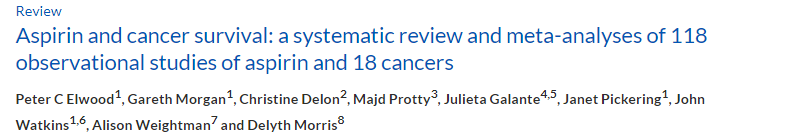
Peter C Elwood et al, Aspirin and cancer survival: a systematic review and meta-analyses of 118 observational studies of aspirin and 18 cancers, ecancermedicalscience (2021). DOI: 10.3332/ecancer.2021.1258
2021年7月2日,卡迪夫大学的学者发表在ecancermedicalscience 上,对 118 项已发表的观察性研究进行了系统评价,在对约 250,000 名癌症患者(包含18种癌症)的治疗方案中服用阿司匹林,死亡风险降低 20%。研究人员甚至比较了阿司匹林对于结肠直癌与其他癌症的死亡率差别。比较显示:
结肠癌的死亡率:
在三次文献检索(2016年、2018年和2020年3月)中发现了24项研究的综合风险比HR:0.72(95%CI:0.63,0.82)。其中,一份报告显示优势比(OR)为0.78。对于全因死亡率,有20项结肠癌研究给出了与阿司匹林相关的综合HR为0.83(95% CI:0.75,0.92)。
15种罕见癌症的死亡率
将其他癌症的18项研究综合在一起观察到癌症死亡率综合HR为0.79(95%CI:0.70,0.88),在5项研究中,综合OR为0.49。而21项研究全因死亡率综合HR为0.67,其中,缺少了HR的5项研究的综合OR为0.47。其他癌症包含鼻咽、消化道癌症,包括口咽、胃、食道和直肠、肝、胆囊的四个部分、胰腺、膀胱、卵巢、子宫内膜、头颈、肺、白血病、胶质瘤、黑色素瘤和两个提出混合癌症。
对于乳腺癌的死亡率,13项研究报告的综合HR 为0.84。有四项研究给出了综合OR为0.75。对于乳腺癌全因死亡率,9项研究的综合HR为0.94。
对于前列腺癌的死亡率,15项研究的综合HR为0.89,其中一项研究中的OR为1.02。对于前列腺癌的全因死亡率来说,7项研究综合HR为1.00,其中一项研究中的OR为1.06。
生存期
研究人员对美国174名患结肠直肠癌的退伍军人进行了跟踪,服用阿司匹林的病人的中位生存期为941天,而未服用阿司匹林的病人的中位生存期为384天。有几篇论文记录了肝癌患者服用阿司匹林后存活率出现提高:其中一篇论文记录了18个月的额外存活率;另一篇论文记录了6%的患者在诊断为癌症后,服用阿司匹林后存活了10年。
利物浦的一个小组用超过44,000名结肠癌患者的数据,得出了一个预测公式,将诊断时的一些因素与生存率联系起来。将一名70岁的非糖尿病男性结肠癌患者的详细资料输入预测公式中,如果加入服用阿司匹林的影响因素,估计生存期会增加5年左右,而女性则增加4年左右。
一项关于子宫内膜癌的研究中,服用阿司匹林的患者中,有91%存活了10年,而不服用阿司匹林的病人有81%存活了10年。
一项对肺癌患者的研究中,服用阿司匹林的患者多存活了1.69年,而不服用阿司匹林的患者仅多存活了1.02年。
一项关于胰腺癌的研究中,服用阿司匹林的患者3年生存率为61%,而未服用阿司匹林的患者3年生存率为26.3%,美国退伍军人头颈部癌症患者的3年生存率为79%,而未服用阿司匹林的患者3年生存率只有56%。
阿司匹林副作用——出血
许多研究报告了使用阿司匹林的病人消化道出血过多。然而,只有极少数报告了致命的出血。在一项研究中,3%服用阿司匹林的患者和3.2%的未服用阿司匹林的病人发生了致命的出血。18,000多名结肠癌患者的队列研究显示,使用阿司匹林的人发生消化道出血的死亡率为0.40%,而不服用阿司匹林的患者为0.36%。经动脉化疗栓塞术治疗的肝癌患者的一项研究称,阿司匹林组有6名患者、非阿司匹林组有7名患者因上消化道出血而死亡。有一篇研究提到,在服用阿司匹林的同时服用质子泵抑制剂(PPI)的患者出血量减少(OR:0.85)。所有提到的出血都与消化道出血有关,没有发现脑出血。
无论是消化道出血还是脑出血,对病人来说都是一种危机,应根据阿司匹林可能带来的益处来评估阿司匹林出血的严重性,此外,还应考虑阿司匹林导致的额外出血的严重性。
原文出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#阿司匹林##癌症#
141
#风险降低#
81
#死亡风险#
78
#癌症患者#
70
可和他汀比高低。
112
#阿司匹林#
274