Lancet oncol:新辅助放化疗治疗食管癌后,内镜超声、活检、PET-CT等方法检测残余病灶的漏诊情况
2018-06-01 MedSci MedSci原创
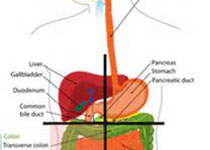
对食管癌进行新辅助放化疗后,约有一半鳞状细胞癌患者的和1/4的腺癌患者在手术前获得病理性完全缓解。因此,对于对新辅助放化疗反应有效的患者,应重新考虑新辅助放化疗后进行标准食管切除术的必要性。近日,Lancet子刊上发表一篇文章,Bo Jan Noordman等人对比新辅助放化疗后,用不同的诊断方法检测残余病灶的准确性,并探究进行临床反应评估的诊断技术的最佳组合。SANO预试验是在荷兰的6个中心开展
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
47
#辅助放化疗#
62
#Lancet#
0
#Oncol#
66
#新辅助#
90
#内镜#
61
#活检#
54
#放化疗#
57
#PET#
65
#漏诊#
64