这次让你看实物!心脏支架、心脏瓣膜、人工血管是什么样子?
2016-12-14 李庆志 李庆志心胸血管大夫
冠状动脉支架,是心脏介入手术中常用的医疗器械,具有疏通动脉血管的作用。心脏支架最早出现在20世纪80年代,经历了金属支架、镀膜支架、可溶性支架的研制历程,主要材料为不锈钢、镍钛合金或钴铬合金。支架实物支架实物支架实物支架植入过程主动脉支架是植入主动脉内治疗主动脉疾病(主动脉夹层、主动脉瘤、主动脉缩窄)的支架,其表面往往覆盖有人工血管膜或人工血管。主动脉覆膜支架各种类型主动脉覆膜支架。手术模式图孙氏
冠状动脉支架,是心脏介入手术中常用的医疗器械,具有疏通动脉血管的作用。心脏支架最早出现在20世纪80年代,经历了金属支架、镀膜支架、可溶性支架的研制历程,主要材料为不锈钢、镍钛合金或钴铬合金。

支架实物
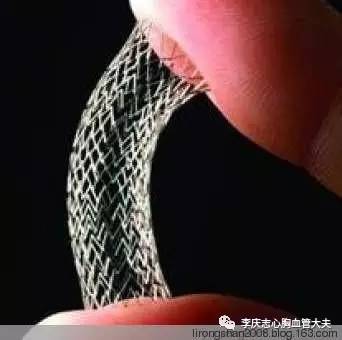
支架实物

支架实物

支架植入过程
主动脉支架是植入主动脉内治疗主动脉疾病(主动脉夹层、主动脉瘤、主动脉缩窄)的支架,其表面往往覆盖有人工血管膜或人工血管。

主动脉覆膜支架

各种类型主动脉覆膜支架。
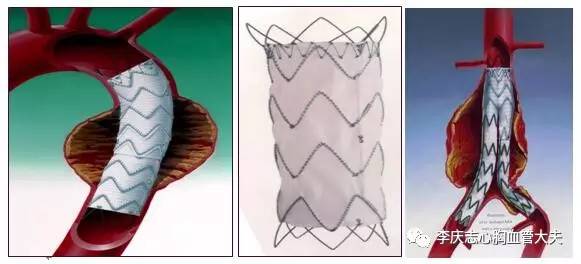
手术模式图

孙氏手术术中支架
心脏人工瓣膜(Heart Valve Prothesis)是可植入心脏内代替心脏瓣膜(主动脉瓣,三尖瓣,二尖瓣),能使血液单向流动,具有天然心脏瓣膜功能的人工器官。当心脏瓣膜病变严重而不能用瓣膜分离手术或修补手术恢复或改善瓣膜功能时,则须采用人工心脏瓣膜置换术。

机械瓣膜实物

机械瓣膜实物,第1、2为单叶瓣,第3、4为双叶瓣
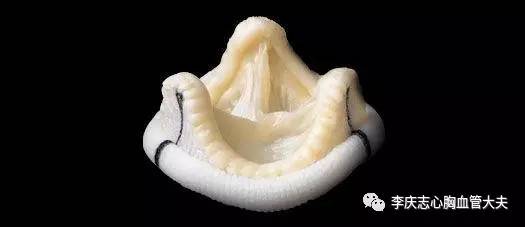
生物瓣

手术过程模式图

介入用的支架瓣膜

介入用的支架瓣膜

各种不同类型支架瓣膜
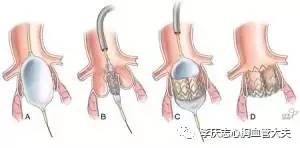
支架瓣膜手术过程

支架瓣膜手术过程
人工血管是许多严重狭窄或闭塞性血管的替代品,多是以尼龙、涤纶(Dacron)、聚四氟乙稀(PTFE)等合成材料人工制造的,适用于全身各处的血管转流术,大、中口径人工血管应用于临床已取得满意的效果。

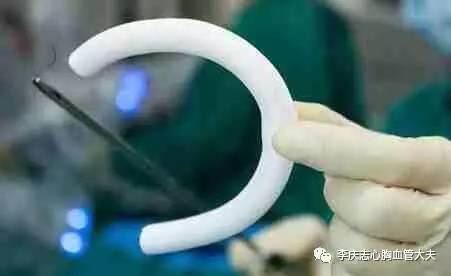
人工血管

带瓣血管

人工血管手术模式图
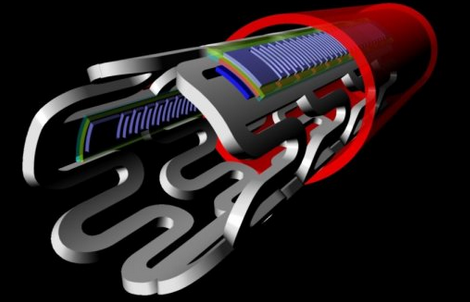
在人体心脏因病损而部分或完全丧失功能而不能维持全身正常循环时,可移植一种用人工材料制造的机械装置以暂时或永久地部分或完全代替心脏功能、推动血液循环,这种装置即人工心脏。

人工心脏

人工心脏

人工心脏植入体内模式图
封堵器作为介入治疗的植入物,用于治疗先天性心脏病:房间隔缺损、室间隔缺损和动脉导管未闭,已在临床得到广泛的应用。主要的原理是将左右心室间的"漏洞"、左右心房间的"漏洞"、主动脉与肺动脉之间的通道堵住。 先心病封堵器分为动脉导管未闭封堵器、房间隔缺损封堵器和室间隔缺损封堵器。
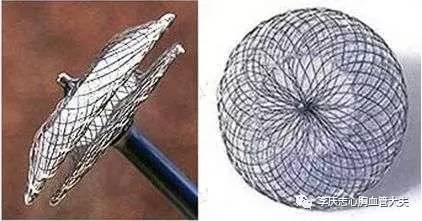
封堵器实物

封堵器实物

封堵器使用过程模式图
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#人工血管#
76
#心脏瓣膜#
73
每一种支架介绍了主要特点,很直观
105
#心脏支架#
68
#瓣膜#
61
第一次这么直观地看
92
作者很用心,让我们更直观的了解和学习,感谢
98
图片内容丰富易解,让外行学习了
84