2018 ASN:美国肾脏病学会肾病周实时资讯--FGF23与磷代谢的全局视角
2018-10-28 MedSci MedSci原创
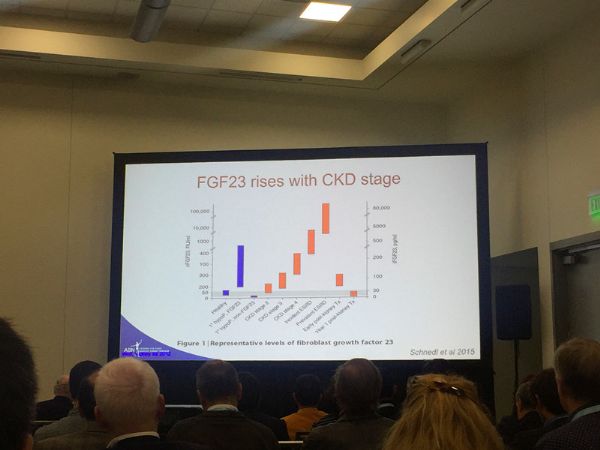
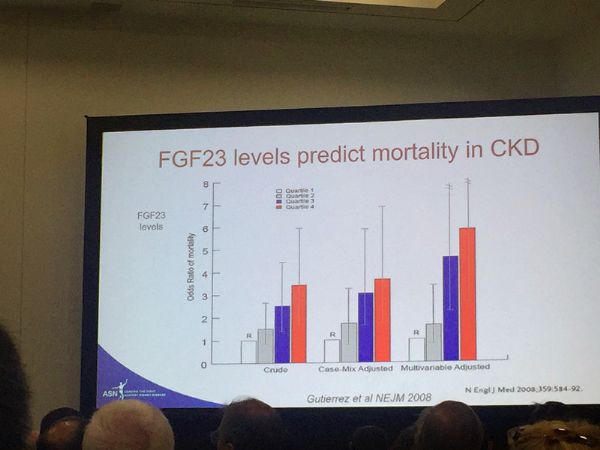
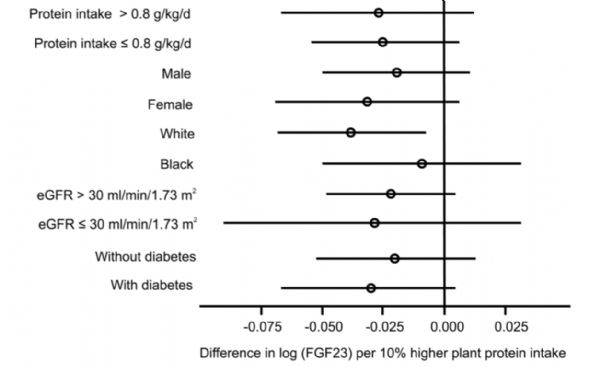
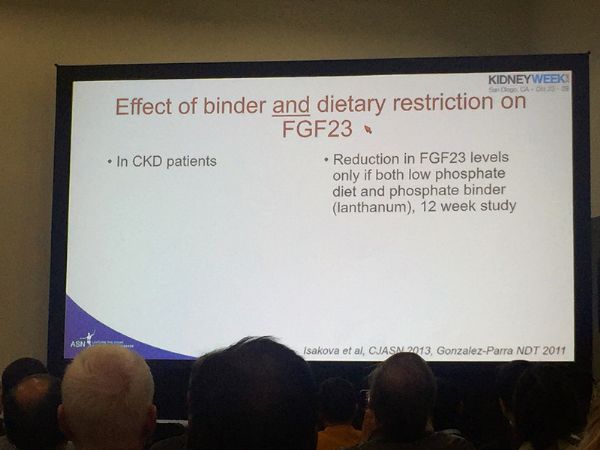
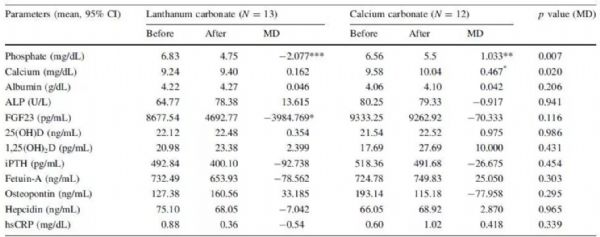
前言2018年ASN(美国肾脏病学会)肾病周已于美国当地时间10月25日正式开幕,本次会议在美国西海岸的海滨城市圣地亚哥举行。ASN肾病周旨在通过专业人员的学术交流,以分享最新的研究进展,推进肾病研究,引领抗击肾脏疾病的斗争。会议上,有关磷代谢关键调节因子FGF23的综合性论述全局性地阐释了FGF23水平与慢性肾病(CKD)患者的疾病进程、死亡率之间的紧密关系,更进一步论述了FGF23水平对C
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#美国肾脏病学会#
135
#FGF23#
108
#ASN#
112
#肾脏病学会#
84
学习了,谢谢分享。
184