European Radiology:DWI对Kaiser评分评估乳腺病变是否有额外价值
2022-07-14 shaosai MedSci原创
乳腺成像报告和数据系统(BI-RADS)被广泛用于乳腺病变的评估,不仅为临床管理提供建议,还为乳腺病变的描述提供了标准术语。
乳腺癌是女性中最常见的癌症,也是与癌症相关的主要死亡原因。影像学在乳腺癌的诊断、随访和治疗评估中起着重要作用,其中动态对比增强磁共振成像(DCE-MRI)为乳腺病变的诊断提供了高分辨率的形态学特征和动力学特征。与乳腺钼靶和超声检查相比,MRI对乳腺癌的检测具有94-100%的高灵敏度。
乳腺成像报告和数据系统(BI-RADS)被广泛用于乳腺病变的评估,不仅为临床管理提供建议,还为乳腺病变的描述提供了标准术语。然而,BI-RADS词典并不是诊断乳腺病变的决策规则。Baltzer等学者在2013年提出了一个新的在机器学习算法的基础上建立的评分系统,名为Kaiser评分(KS)。 KS实际上是一个基于BI-RADS标准的决定性树状结构,即根征(或尖征)、时间信号强度曲线(TIC)的类型、边缘、内部增强模式和水肿。引入KS后,在一些使用外部数据的研究证实了其对乳腺病变特征诊断的价值。与BI-RADS词典相比,KS为临床上乳腺病变的定性提供了一个简单而直观的决策规则,且准确性较高。
然而,KS仅基于乳腺DCE-MRI图像,例如扩散加权成像(DWI)等功能成像没有参与KS的组成。
近日,发表在European Radiology杂志的一项研究探讨了DWI对提高KS评估乳腺病变中诊断性能的价值,为建立一个规范化的乳腺病变的评估标准提供了参考依据。
本研究于2015年1月-2019年12月纳入了246名患者的共273个病变(155名恶性肿瘤),所有病变均经病理学证明。由两位对病理结果保密的放射科医生根据KS对病变进行评估。评分>4的病变被认为是恶性的。使用ADC值的四个阈值-1.3×10-3mm2/s、1.4×10-3mm2/s、1.53×10-3mm2/s和1.6×10-3mm2/s进行良性和恶性病变的区分。对于合并诊断,KS>4且ADC值低于预设临界值的病变被认为是恶性的;反之则为良性的。比较了KS、DWI和联合诊断的敏感性、特异性和曲线下面积(AUC)。
KS的AUC明显高于单独使用DWI(0.941 vs 0.901,P = 0.04)。KS(96.8%)和DWI(97.4 - 99.4%)的敏感性相当(p > 0.05),而KS(83.9%)的特异性明显高于DWI(19.5-56.8%)(p < 0.05)。添加DWI作为KS的辅助检查,使特异性增加0-2.5%,敏感性降低0.1-1.3%;但是,差异没有达到统计学意义(P > 0.05)。
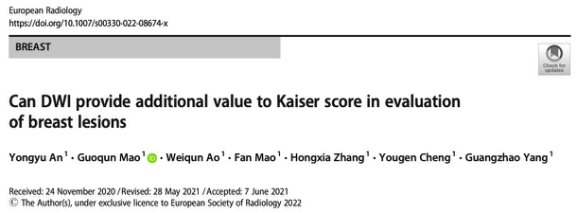
图 53岁女性,左乳有可触及的肿块。MRI显示一个19毫米的肿块,边缘光滑,内部均匀强化,并有廓清现象,对应的Kaiser评分为4分。结合Kaiser评分和DWI显示真阴性的发现
本研究显示,KS在区分乳腺良性和恶性病变方面取得了较高的诊断性能,且比单独使用DWI的性能更好,而将DWI加入KS的评估中并不能显著提高KS的诊断性能。
原文出处:
Yongyu An,Guoqun Mao,Weiqun Ao,et al.Can DWI provide additional value to Kaiser score in evaluation of breast lesions.DOI:10.1007/s00330-022-08674-x.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
73
#AIS#
82
#DWI#
93
感谢分享
0