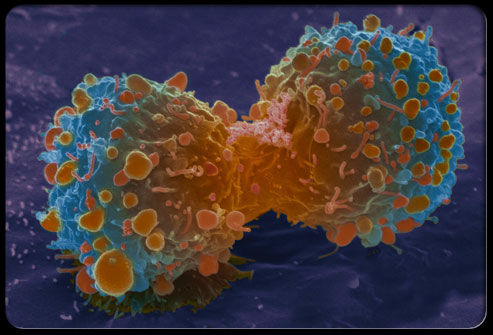
JAMA:绝经后激素干预对女性乳腺癌发病率及死亡率的影响
2020-07-29 MedSci原创 MedSci原创
长期随访发现,对于子宫切除的绝经后女性,接受结合雌激素可降低乳腺癌发病率和死亡率,但对于保留子宫的参与者,激素干预会增加乳腺癌发病率
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#发病率#
61
#癌发病率#
92
#绝经后激素#
63
#癌发病#
85
学习
133
#绝经#
59
#绝经后#
66
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
89
学习了
126