Carcinogenesis:核受体Nur77相关癌症信号转导研究中获进展
2012-01-06 MedSci原创 MedSci原创
近日,国际著名杂志Carcinogenesis刊登了厦门大学生命科学学院的吴乔教授研究团队的最新研究成果“Orphan receptor TR3 participates in cisplatin-induced apoptosis via Chk2 phosphorylation to repress intestinal tumorigenesis。”,吴乔教授的主要研究领域是核受体的作用机理
近日,国际著名杂志Carcinogenesis刊登了厦门大学生命科学学院的吴乔教授研究团队的最新研究成果“Orphan receptor TR3 participates in cisplatin-induced apoptosis via Chk2 phosphorylation to repress intestinal tumorigenesis。”,吴乔教授的主要研究领域是核受体的作用机理和细胞信号转导调控、以核受体为靶点的抗肿瘤和代谢性疾病药物研究。
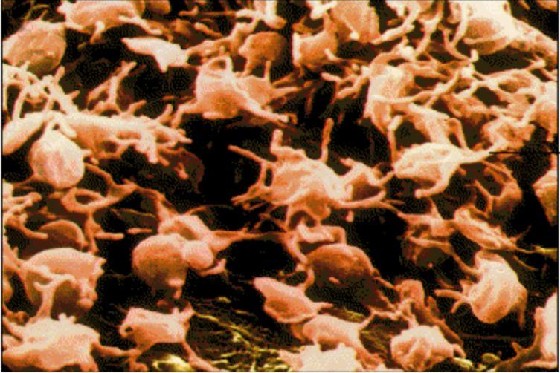
孤儿受体是指一类目前还未发现其相应配体的核受体,这些受体能和特定DNA上的应答元件结合,调控特定基因的表达,从而在细胞的生长、分化和凋亡等生物学过程中发挥重要的调节作用。TR3也被称为Nur77,是一种立刻早期基因(immediateearlygene)的产物,与固醇类激素受体结构相似,是核受体超家族的重要成员之一,可被血清及表皮生长因子、神经生长因子、血小板生长因子等诱导表达,具有复杂的生物学功能,涉及细胞增殖、分化发育和凋亡等过程。
在这论文中,研究人员发现现在肿瘤治疗一线药物顺铂刺激下,核孤儿受体TR3发生磷酸化修饰,并在肠癌细胞的凋亡过程中发挥重要作用。机理分析表明,顺铂首先激活细胞周期检控点激酶Chk2,TR3的T88位点在该激酶的作用下发生磷酸化,蛋白稳定性增强,同时,发生磷酸化修饰的TR3还能够募集转录辅抑制因子N-CoR,通过结合到下游基因BRE和RNF-7 promoter的TR3应答元件上,下调这些抗凋亡基因的表达,从而诱导肠癌细胞凋亡。在小鼠模型中也观察到敲除TR3基因后,顺铂对Apcmin/+小鼠肠道肿瘤或裸鼠移植瘤的抑制效果被明显地削弱。
该研究发现了顺铂通过TR3介导来诱导肿瘤细胞凋亡的新途径,为肠癌的治疗提供了新的药物靶点。
此外,今年10月吴乔课题组研究人员在Onocogene杂志上发表了另一篇研究论文,证实了Pin1对TR3异构化修饰是TR3发挥其促细胞增殖功能的前提,从而为癌症治疗提供了一个潜在的新靶点。而在8月发表于国际SCI源刊物《GUT》的文章中,揭示了孤儿受体TR3通过负调控Wnt信号通路活性抑制结肠癌发生的分子机理。该研究从分子、细胞、小鼠和临床水平证实了TR3可以作为结肠癌治疗的一个潜在靶点,TR3激动剂则可能成为治疗结肠癌的潜在药物。(生物谷Bioon.com)
Orphan receptor TR3 participates in cisplatin-induced apoptosis via Chk2 phosphorylation to repress intestinal tumorigenesis
Lu-ming Yao1, Jian-ping He1, Hang-zi Chen, Yuan Wang, Wei-jia Wang, Rong Wu, Chun-dong Yu and Qiao Wu*
Cisplatin is a widely used antitumor agent that induces aggressive cancer cell death via triggering cellular proteins involved in apoptosis. Here, we demonstrate that cisplatin effectively induces orphan nuclear receptor TR3 phosphorylation by activating Chk2 kinase activity and promoting cross-talk between these two proteins, thereby contributing to the repression of intestinal tumorigenesis via apoptosis. Mechanistic analysis has demonstrated that Chk2-induced phosphorylation enables TR3 to bind to its response elements on the promoters of the BRE and RNF-7 genes, leading to the negative regulation of these two anti-apoptotic genes. Furthermore, the induction of apoptosis by cisplatin is mediated by TR3, and knock-down of TR3 reduces cisplatin-induced apoptosis in colon cancer cells by 27%. The role of TR3 in cisplatin chemotherapy was further clarified in mouse models. In Apcmin/+ mice, cisplatin inhibits intestinal tumorigenesis by 70% in a TR3 phosphorylation-dependent manner; however, the loss of TR3 function in Apcmin/+/TR3-/- mice leads to the failure of cisplatin-induced repression of tumorigenesis. Consistently, xenografts derived from TR3 knock-down colon cancer cells are insensitive to cisplatin treatment, whereas a significant curative effect (50% inhibition) is observed in xenografts with functional TR3. Taken together, our study reveals a novel cross-talk between Chk2 and TR3 and sheds light on the mechanism of cisplatin-induced apoptosis through TR3. Therefore, TR3 may be a new target of cisplatin for colon cancer therapy.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Carcinogenesis#
87
#核受体#
69
#CIN#
61
#Gene#
69
#ESI#
64