下颌喙突异位智齿含牙囊肿伴感染1例
2019-09-08 单忠艳 刘子艺 胡延佳 北京口腔医学
患者,男,51岁,2017年7月因左侧后牙牙龈反复肿痛10年,加重1个月入院。专科检查示:患者面部对称无畸形,开口度一指,左侧下颌骨下颌支内侧压痛,关节区无压痛,恒牙31颗,排列整齐,口内未见38萌出,影像学检查:全景片示:左侧下颌骨喙突部见边缘光滑的类圆形透射影,内含有埋伏牙,形似磨牙,牙冠朝向囊腔。锥形束CT示左侧喙突见圆形低密度影,周围见骨白线,囊内见一牙齿,冠部朝向囊腔(图1,2)
牙齿异位是指牙齿位于除牙槽弓以外的颌骨或其他区域。牙齿异位虽非常少见,但也有牙齿异位于下颌骨髁突、乙状切迹、上颌窦、鼻、翼腭窝、颞下间隙、颊间隙及咽旁间隙的病例报道。磨牙异位于喙突国内外报道不到20例。喙突区含牙囊肿国内外报道不到3例。我院诊治1例左侧下颌骨喙突部异位智齿伴感染性含牙囊肿,报道如下。
1.临床资料
患者,男,51岁,2017年7月因左侧后牙牙龈反复肿痛10年,加重1个月入院。专科检查示:患者面部对称无畸形,开口度一指,左侧下颌骨下颌支内侧压痛,关节区无压痛,恒牙31颗,排列整齐,口内未见38萌出,影像学检查:全景片示:左侧下颌骨喙突部见边缘光滑的类圆形透射影,内含有埋伏牙,形似磨牙,牙冠朝向囊腔。锥形束CT示左侧喙突见圆形低密度影,周围见骨白线,囊内见一牙齿,冠部朝向囊腔(图1,2)。

图1 术前全影片

图2 冠状位CBCT影像
2.治疗与结果
全身麻醉下,做下颌升支前缘切口,于下颌骨表面剥离,见下颌骨内侧壁骨质已破坏,用咬骨钳去除病变骨质,完整剥离囊壁及含牙,术中见囊液呈黄褐色,浑浊(图3)。彻底止血后,生理盐水冲洗创面,将引流条填入骨腔,缝合,固定引流条,冲洗口腔。术后将囊壁送病理检查,病理报告为下颌骨含牙囊肿并伴有感染。术中刮治的囊壁和拔除的埋伏牙,埋伏牙含有4个牙尖,形似下颌磨牙,牙冠色黑,牙冠釉质似缺如,牙根发育完全,为融合根(图3)。
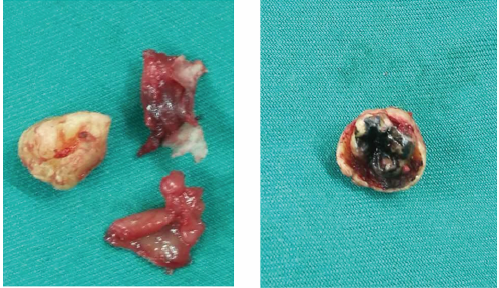
图3 术后标本
3.讨论
下颌智齿异位却并不常见。有文献报道下颌智齿异位于下颌髁突、下颌乙状切迹、翼下颌间隙以及下颌升支。但是下颌智齿异位于喙突部的病例少见。牙齿异位的病因,目前尚不完全清楚,在牙齿发育过程中,上皮与间充质相互作用的过程遭到破坏可能会导致牙齿的异位发育和萌出。
含牙囊肿是在釉质发育完成后,由于釉牙骨质界处的上皮衬里发育缺陷引起,因此含牙囊肿的发生可能与牙齿的异位有关,有文献报道在影像上可以看到从下颌牙弓区延伸到牙齿异位区的透射路径,这个路径可能提示牙齿移动的过程是从牙槽弓区开始,结束于异位区。回顾文献,磨牙异位于喙突部可以无任何临床表现,也可因导致面部肿胀、疼痛、口腔异味、开口受限等症状来求诊。本病例主要表现为后牙牙龈反复肿痛。异位于喙突部的下颌第三磨牙且伴有含牙囊肿的病例罕见,怀疑为异位牙时,应做影像学检查。
原始出处:
单忠艳,刘子艺,胡延佳,全宏志.下颌喙突异位智齿含牙囊肿伴感染1例[J].北京口腔医学,2018,26(05):289-290.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#下颌#
62
#囊肿#
59
#智齿#
65