J Hepatol:肝细胞NRF2特异性激活调控肝纤维化和肝癌的发生
2021-01-23 MedSci原创 MedSci原创
KEAP1/NRF2系统在肝纤维化和肝癌的发生发展中有什么样的作用呢?
在慢性肝病中,炎症诱导氧化应激,从而可能导致肝损伤、纤维化和癌变进展。KEAP1/NRF2轴是细胞氧化还原平衡的主要调节因子。在本研究中,研究人员调查了KEAP1/NRF2系统是否与人和小鼠的肝病进展有关。
研究人员对63例非酒精性脂肪性肝病患者进行了肝组织RNA测序,以研究氧化应激与组织学和临床参数的相关性。为了进行功能分析,研究人员将肝细胞NEMO基因特异性敲除(NEMO△hepa)小鼠与肝细胞特异性Keap1基因敲除(KEAP1△hepa)小鼠杂交。
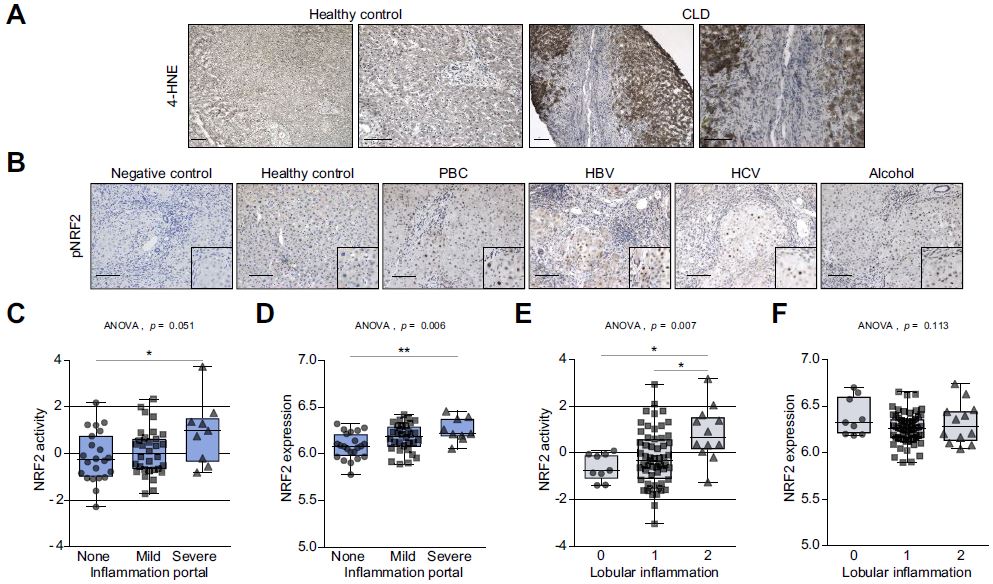
慢性肝病患者肝组织氧化应激增强、NRF2激活
人肝组织切片的免疫组化分析显示,慢性肝病患者肝组织中的氧化应激增强、NRF2高表达。一个NAFLD儿童队列中的肝脏样本的RNA测序显示,NRF2激活显著增强与炎症级别相关,但与脂肪变性的级别无关,该结果在另一个成人NASH队列中得到了证实。
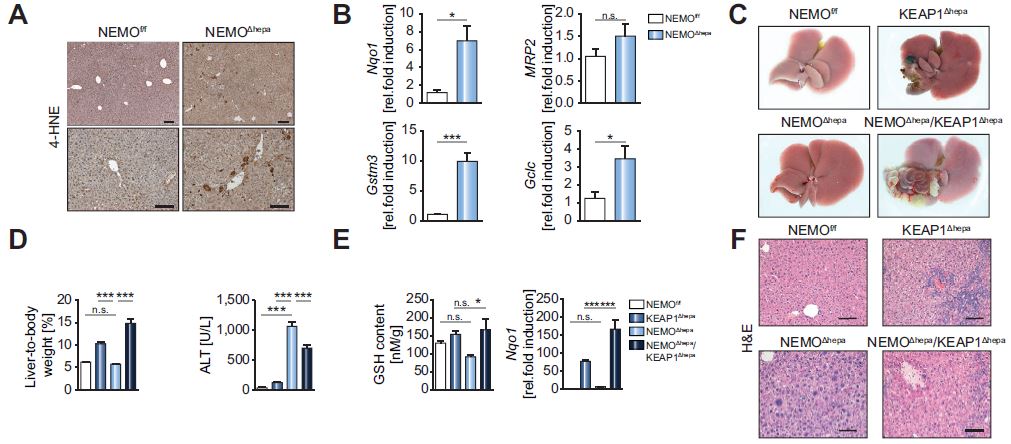
在脂肪肝小鼠中,氧化应激增强与NRF2靶基因激活相关
在小鼠中,微阵列分析显示,Keap1缺失可诱导NRF2靶基因参与谷胱甘肽代谢和异种应激(如,Nqo1)。此外,敲除Keap1后还可挽救NEMO△hepa肝脏中最重要的抗氧化剂缺陷之一,谷胱甘肽(GSH)。
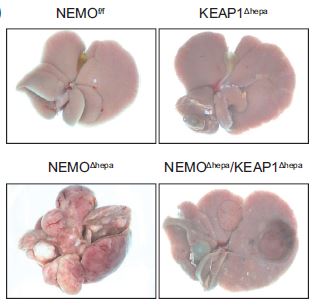
NEMO△hepa/Keap1△hepa小鼠的肝纤维化和肝癌进展延缓
此外,与NEMO△hepa肝脏相比,NEMO△hepa/Keap1△hepa肝脏的细胞凋亡减少,与细胞周期调节和DNA复制相关的基因的表达也显著下调。与NEMO△hepa肝脏相比,NEMO△hepa/Keap1△hepa显示出纤维化形成减少、肿瘤发病率降低、肿瘤数量减少和肿瘤体积缩小。
综上,非酒精性脂肪性肝炎患者的NRF2激活与炎症程度相关,而与脂肪变性无关。对小鼠的功能分析表明,在慢性肝病中NRF2激活可通过减轻肝细胞癌的形成、发生和发展而起到保护作用。
原始出处:
Mohs Antje,Otto Tobias,Schneider Kai Markus et al. Hepatocyte-specific NRF2 activation controls fibrogenesis and carcinogenesis in steatohepatitis. J Hepatol, 2020, 10.1016/j.jhep.2020.09.037.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肝纤维#
90
#肝细胞#
86
#特异性#
67
#Nrf2#
133
#EPA#
78
#肝癌#
232
好资料
130
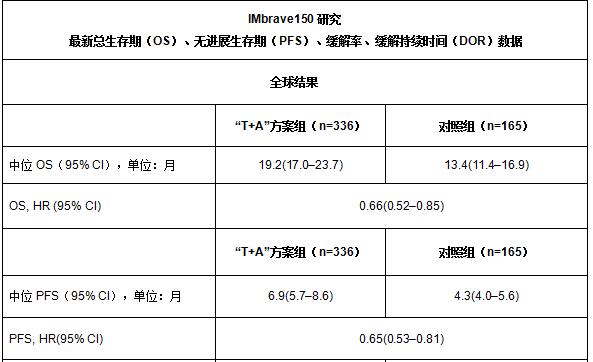
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
113
学习了
121